Translate this page into:
Knowledge and attitude gap toward ear, nose, and throat foreign bodies in children among parents and teachers in Federal Capital Territory

*Corresponding author Enoch Auta Dahilo, Department of Otorhinolaryngology, University of Abuja/University of Abuja Teaching Hospital, Gwagwalada, Nigeria. edahiloa@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Dahilo EA, Yikawe SS, Omosule IE, Folorunso DF. Knowledge and attitude gap toward ear, nose, and throat foreign bodies in children among parents and teachers in Federal Capital Territory. Ann Med Res Pract. 2024;5:2. doi: 10.25259/ANMRP_11_2023
Abstract
Objectives:
Ear, nose, and throat (ENT) foreign bodies (FBs) are common Otorhinolaryngological emergencies, especially among children. This study aims to assess the knowledge and attitude gap towards ENT FBs in children among parents and teachers, with a view to advocating public enlightenment on the dangers of ENT FBs in children. This study aims to assess the knowledge and attitude gap toward ENT FBs in children among parents and teachers with a view to advocating public enlightenment on the dangers of ENT FBs.
Material and Methods:
This was a cross-sectional descriptive prospective study. A multistage sampling method was used to enroll participants among the six Area Councils in the Federal Capital Territory. Participants were among parents and guardians whose children attended those schools. The instrument for data collection was a pre-tested, standardized, and semi-structured questionnaire.
Results:
Of the 270 questionnaires issued, there were only 240 responses, which consisted of 29 parents and 211 teachers. Among the teachers, there were 128 females (60.7%) and 83 males (39.3%) M: F 1:1.5. Majority of them were 30–39 years 102 (51.2%). Most of the parents were between 30 and 39 years 14 (48.3%).
Conclusion:
Awareness creation among the parents and teachers is fundamental to bridge the attitude gap in our society.
Keywords
Foreign bodies
Children
Parents and teachers
INTRODUCTION
Ear, nose, and throat (ENT) foreign bodies (FBs) are common Otorhinolaryngological emergencies.[1,2] They account for 11–30% of Otorhinolaryngological emergencies.[3] FBs in the ENT could be living and non-living. Among the non-living, they could be organic and inorganic.[1,3,4] The effect of FBs on children varies, ranging from mere discomfort to a life-threatening emergency.[2,5,6] ENT FBs are more common among children under five years of age[5,6] for various reasons. This includes curiosity, imitation, boredom, the need to explore orifices, mental retardation, and fun-seeking.[2,3,5] Otorhinolaryngologists, Pediatricians, and Emergency and Primary Care Physicians are the Specialists that usually attend to these patients.[1,3,4]
Ibekwe et al. conducted a retrospective study among 202 pediatric patients who presented to the emergency with various injuries; 181 had FB injuries, with a male-to-female ratio of 1.1:1. Most of these patients were three years old. The most common site was the nasal cavity (48.62%), followed by the ear with the insertion of beads (28.17%). They found up to 23 patients required a tracheostomy as part of their treatment.[7] Adedeji et al. found a prevalence of 5.7% among all the ENT cases seen in adults and children, and most of the cases were found in children under five years of age. In addition, most of the FBs were found in the ear. It was, however, noted that the most frequent foreign material seen were seeds.[8]
In other regions, authors have published findings similar to the ones in Nigeria.[9] In a hospital-based study by Awad and El-Taher,[3] they found a prevalence of 30%, most common among boys within the age of 6 years. The majority had FBs in the aerodigestive tract, followed by aural, nasal, and airway FB inhalation. Mukherjee et al. also found a male preponderance with a mean age of about five years in their study. Most of the foreign material was found in the nose. They also found that poor educational background, low socioeconomic status, and being a child of a housewife were significantly associated with FB insertion in children.[5] Loperfido et al. also found a male preponderance and a mean age of 5.5 years in their study, consisting of a sample size of 1623 children. The foreign materials were most common in the ear, followed by the nose, pharynx, mouth, and airway.[10] A study done in Malaysia by Chai et al. with 1084 children also had similar findings. The most common site was the ear, followed by the nose, pharynx, and esophagus.[6]
All sorts of FBs can be found in children. These range from food particles such as nuts, seeds, food bolus, bones, and sweets to non-food particles such as beads, batteries, small toy parts, biro parts, and any small material that they can lay their hands on.[1,3,5,7-10]
The symptoms depend on the site where the foreign materials are found. An FB might present in the ear with no symptoms, pain, signs of inflammation, or hearing impairment.[8] In the throat or food passage, it may present irritability, drooling of saliva, sudden onset of cough, and choking spells.[3,8] FBs in the nose may present with unilateral foul-smelling rhinorrhea, epistaxis, and nasal blockage, and it may get dislodged into the esophagus or airway, requiring emergency removal under general anesthesia.[9,10]
Most FBs can be removed in the clinic, as reported by Adedeji et al. All FBs in the ear and nose were removed in the clinic without anesthesia. For FB in the throat, only nine out of 25 had to be removed under general anesthesia; the remaining were removed in a clinic by the ENT nurses (85%) and family Physicians (8%).[8] Loperfido et al. also has more cases of FBs addressed in the clinic (1049), while few (35) had surgical intervention in the theater.[10] Hira et al. reported septal perforation and epistaxis as complications noted after nasal FB removal.[9]
Children spend most of their time at home with their parents or in school with their teachers. Therefore, the first “diagnosis” of FB insertion/ingestion/aspiration is made by either the parent/caregiver or the teacher. Schools are environments where children from different backgrounds come together for learning, play, and social interaction.[11,12] Younger children need close supervision and constant attention. As such, the teacher often assumes multiple roles of teaching, caregiving, and, in some instances, the administration of first aid in medical emergencies.[11-13] In some schools, the number of students may overwhelm the teacher, whose attention is already fixed on imparting knowledge to the students. This may mean that the teacher may be unable to detect that a child has inserted an FB or immediately give the child appropriate attention. Parental attention is also vital in early intervention in cases of ENT FBs in children. Older children may report insertion of FBs, but younger children may only present with signs that may suggest an FB has passed into the ear, nose, or throat.[3]
The knowledge, attitudes, and practices (KAP) of parents and teachers regarding ENT FBs in children are important factors influencing the prevention, diagnosis and treatment of these cases. Parents and teachers are often the first to notice or suspect ENT FBs in children and decide whether to seek medical help or attempt to remove them by themselves. Their KAP may affect the type, location, duration, and complication of ENT FBs in children. Therefore, it is important to study parents’ and teachers’ KAPs regarding ENT FBs in children, as they are the primary caregivers and educators of this age group. This study aims to assess the level of KAP of parents and teachers. However, there are insufficient studies on the KAP of parents and teachers regarding ENT FBs in children in our environment. Most previous studies have focused on the clinical aspects of ENT FBs, such as their presentation, characteristics, management, and outcomes. Therefore, this study aims to assess the KAP of parents and teachers regarding ENT FBs in children and to identify the factors associated with them.
MATERIAL AND METHODS
This was a cross-sectional descriptive and prospective study conducted among teachers in various schools in the Federal Capital Territory (FCT) and among parents/guardians whose children/wards attend those schools. The instrument for data collection was a pre-tested, standardized, and semi-structured questionnaire. The questionnaire consisted of four sections: Sociodemographic profile of participants, KAP sessions. Before the administration of the questionnaire, consent was obtained from participants.
A multistage sampling method was used to enroll participants. Among the six Area Councils in the FCT, three were randomly selected (stage 1). From each of the selected Area Councils, three wards (a total of nine wards were selected) were randomly selected (stage 2). In each of the selected wards, two schools (1 private and one government) were selected, making a total of 18 selected schools selected (stage 3). In each selected school, ten teachers and five parents were randomly selected to participate in the study (totaling 270 participants). Random sampling was carried out by a process of balloting.
The inclusion criteria were teachers who taught in primary and junior secondary schools within the FCT and parents/guardians whose child/ward attended the schools. Parents/ guardians and teachers who did not consent were excluded from the study. Data were analyzed using the Statistical Package for the Social Sciences version 24. Responses of the participants to items on the questionnaire were scored on each point, and summary counts were expressed in percentages. Correct responses were scored one mark, while wrong and non-responses were scored zero. Statistical significance was set at a 95% confidence level and a = 0.05.
RESULTS
There were 240 responses (29 parents and 211 teachers) out of the 270 questionnaires.
Teachers’ KAP
Among the teachers, there were 128 females (60.7%) and 83 males (39.3%) M: F 1:1.5. Majority of them were 30–39 years 102 (51.2%), followed by 40–49, which were 44 (20.9%), as shown in Table 1.
| Sex | ||
|---|---|---|
| Male | 83 | 39.3 |
| Female | 128 | 60.7 |
| Age group (years) | ||
| 20–29 | 35 | 16.6 |
| 30–39 | 108 | 51.2 |
| 40–49 | 44 | 20.9 |
| 50–59 | 22 | 10.4 |
| ≥60 | 2 | 0.9 |
Table 2 shows the teachers’ education level and the category of students being taught. Most teachers (70.6%) have a tertiary level of education and are secondary school teachers.
| Level of education | ||
|---|---|---|
| Secondary | 11 | 5.2 |
| Tertiary | 149 | 70.6 |
| Postgraduate | 47 | 22.3 |
| Others | 4 | 1.9 |
| Category of students you are teaching | ||
| Pre-nursery | 17 | 8.1 |
| Nursery | 20 | 9.5 |
| Primary | 62 | 29.4 |
| Secondary | 110 | 52.1 |
| Others | 2 | 0.9 |
In terms of teaching experience, most of the teachers have taught for more than ten years (45%). In addition, most teach in privately owned schools in the Gwagwalada area council of Abuja, as shown in Table 3.
| Number of years in practice | ||
|---|---|---|
| <5 | 40 | 19.0 |
| 5–9 | 55 | 26.0 |
| ≥10 | 95 | 45.0 |
| Not specified | 21 | 10.0 |
| Area council of practice | ||
| Municipal | 25 | 11.8 |
| Gwagwalada | 116 | 55.0 |
| Kwali | 50 | 23.7 |
| Kuje | 18 | 8.5 |
| Abaji | 1 | 0.5 |
| Bwari | 1 | 0.5 |
| Type of school | ||
| Government-owned | 93 | 44.1 |
| Private owned | 107 | 50.7 |
| Others | 11 | 5.2 |
KAP
Figure 1 shows teachers’ KAPs on ENT FBs. One hundred and six (50.2%) had poor knowledge compared to 49.8% with good knowledge.
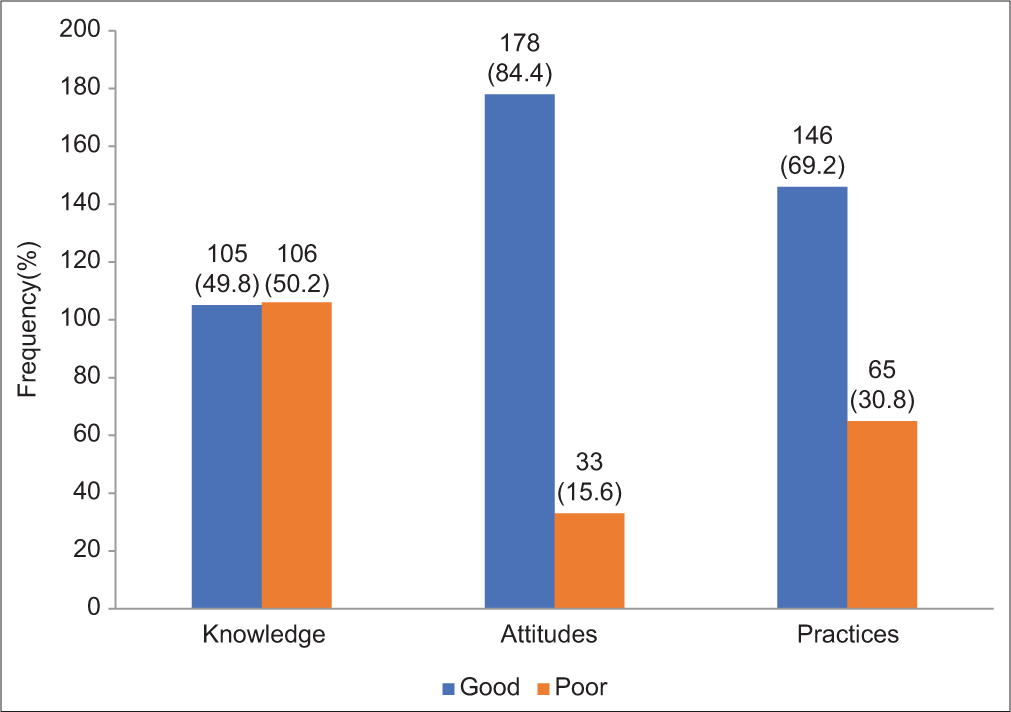
- Knowledge attitudes and practices of teachers.
However, they showed good attitude (84.4%) and practice (69.2%), with only (15.6%) and (30.8%) showing poor attitudes and poor practice, respectively [Figure 1].
There was no significant association between the sex (P = 0.932), age group (P = 0.062), level of education (P = 0.066), category of students taught (P = 0.969), number of years in practice as a teacher (P = 0.360), or location among our study population (0.604) [Table 4].
| Variables | Knowledge | χ2 | P-value | |
|---|---|---|---|---|
| Good n=105 n (%) | Poor n=106 n (%) | |||
| Sex | ||||
| Male | 41 (39.0) | 42 (39.6) | 0.007 | 0.932 |
| Female | 64 (61.0) | 64 (60.4) | ||
| Age group (years) | ||||
| 20–29 | 13 (12.4) | 22 (20.8) | 8.983 | 0.062 |
| 30–39 | 53 (50.5) | 55 (51.9) | ||
| 40–49 | 23 (21.9) | 21 (19.8) | ||
| 50–59 | 16 (15.2) | 6 (5.7) | ||
| ≥60 | 0 (0.0) | 2 (1.9) | ||
| Education | ||||
| Secondary | 3 (2.9) | 8 (7.6) | 7.193 | 0.066 |
| Tertiary | 71 (67.6) | 78 (73.6) | ||
| Postgraduate | 30 (28.6) | 17 (16.0) | ||
| Others | 1 (1.0) | 3 (2.8) | ||
| Category of students being taught | ||||
| Pre-nursery | 8 (7.6) | 9 (8.5) | 0.549 | 0.969 |
| Nursery | 9 (8.5) | 11 (10.4) | ||
| Primary | 33 (31.5) | 29 (27.4) | ||
| Secondary | 54 (51.4) | 56 (52.8) | ||
| Others | 1 (1.0) | 1 (0.9) | ||
| Number of years in practice | ||||
| <5 | 16 (17.0) | 24 (25.0) | 2.044 | 0.360 |
| 5–9 | 30 (31.9) | 25 (26.0) | ||
| ≥10 | 48 (51.1) | 47 (49.0) | ||
| Area council of practice | ||||
| Municipal | 12 (11.4) | 13 (12.3) | 3.626 | 0.604 |
| Gwagwalada | 55 (52.4) | 61 (57.5) | ||
| Kwali | 29 (27.6) | 21 (19.9) | ||
| Kuje | 9 (8.6) | 9 (8.5) | ||
| Abaji | 0 (0.0) | 1 (0.9) | ||
| Bwari | 0 (0.0) | 1 (0.9) | ||
| Area council of domicile | ||||
| Municipal | 15 (14.3) | 11 (10.4) | 2.400 | 0.663 |
| Gwagwalada | 55 (52.4) | 63 (59.5) | ||
| Kwali | 25 (23.7) | 19 (17.9) | ||
| Kuje | 9 (8.6) | 12 (11.4) | ||
| Bwari | 1 (1.0) | 1 (0.9) | ||
| Type of school | ||||
| Government-owned | 46 (43.8) | 47 (44.3) | 0.106 | 0.948 |
| Private owned | 54 (51.4) | 53 (50.0) | ||
| Others | 5 (4.8) | 6 (5.7) | ||
χ2 Chi-square test statistic
The Chi-square test for association also showed no significant association between the sex (P = 0.097), age group (P = 0.631), level of education (P = 0.777), category of students taught (P = 0.382), number of years in practice as a teacher (P = 0.584), or location among our study population (P = 0.231)
Comparing the sociodemographics of the teachers with their practices, sex (P = 0.097), age group (P = 0.631), level of education (P = 0.777), category of students taught (P = 0.382), number of years in practice as a teacher (P = 0.584), or location among our study population (P = 0.231) [Table 5].
| Variables | Practices | χ2 | P-value | |
|---|---|---|---|---|
| Good n=146 n (%) |
Poor n=65 n (%) |
|||
| Sex | ||||
| Male | 52 (35.6) | 31 (47.7) | 2.749 | 0.097 |
| Female | 94 (64.4) | 34 (52.3) | ||
| Age group (years) | ||||
| 20–29 | 27 (18.5) | 8 (12.3) | 2.575 | 0.631 |
| 30–39 | 71 (48.6) | 37 (56.9) | ||
| 40–49 | 31 (21.2) | 13 (20.0) | ||
| 50–59 | 15 (10.3) | 7 (10.8) | ||
| ≥60 | 2 (1.4) | 0 (0.0) | ||
| Education | ||||
| Secondary | 8 (5.5) | 3 (4.6) | 1.101 | 0.777 |
| Tertiary | 105 (71.9) | 44 (67.7) | ||
| Postgraduate | 31 (21.2) | 16 (24.6) | ||
| Others | 2 (1.4) | 2 (3.1) | ||
| Category of students being taught | ||||
| Pre-nursery | 13 (8.9) | 4 (6.2) | 4.185 | 0.382 |
| Nursery | 16 (11.0) | 4 (6.2) | ||
| Primary | 46 (31.5) | 16 (24.6) | ||
| Secondary | 70 (47.9) | 40 (61.5) | ||
| Others | 1 (0.7) | 1 (1.5) | ||
| Number of years in practice | n=132 | n=58 | ||
| <5 | 30 (22.8) | 10 (17.2) | 1.076 | 0.584 |
| 5–9 | 39 (29.5) | 16 (27.6) | ||
| ≥10 | 63 (47.7) | 32 (55.2) | ||
| Area council of practice | ||||
| Municipal | 14 (9.6) | 11 (16.9) | 6.867 | 0.231 |
| Gwagwalada | 86 (58.9) | 30 (46.2) | ||
| Kwali | 30 (20.5) | 20 (30.8) | ||
| Kuje | 14 (9.6) | 4 (6.2) | ||
| Abaji | 1 (0.7) | 0 (0.0) | ||
| Bwari | 1 (0.7) | 0 (0.0) | ||
| Area council of domicile | ||||
| Municipal | 14 (9.6) | 12 (18.5) | 7.144 | 0.128 |
| Gwagwalada | 86 (58.9) | 32 (49.2) | ||
| Kwali | 27 (18.5) | 17 (26.2) | ||
| Kuje | 17 (11.6) | 4 (6.2) | ||
| Bwari | 2 (1.4) | 0 (0.0) | ||
| Type of school | ||||
| Government-owned | 61 (41.8) | 32 (49.2) | 8.254 | 0.016* |
| Private owned | 81 (55.5) | 26 (40.0) | ||
| Others | 4 (2.7) | 7 (10.8) | ||
Parents’ KAP
The number of parents who had a valid response was 29 [Table 6].
| Sex | ||
| Male | 6 | 20.7 |
| Female | 23 | 79.3 |
| Age group (years) | ||
| 20–29 | 3 | 10.3 |
| 30–39 | 14 | 48.3 |
| 40–49 | 7 | 24.1 |
| 50–59 | 5 | 17.2 |
| ≥60 | 3 | 10.3 |
Most of the parents attained a tertiary level of education 16 (55.2%), and most of them were civil servants 14 (48.3%), who also resided in Gwagwalada area council of the FCT.
Overall, the parents had good knowledge 17 (58.6%), attitude 25 (86.2%), and practice 19 (65.5%) [Table 7].
| Level of education | ||
| Secondary | 1 | 3.4 |
| Tertiary | 16 | 55.2 |
| Postgraduate | 11 | 37.9 |
| Others | 1 | 3.4 |
| Parent’s occupation | ||
| Civil servant | 14 | 48.3 |
| Public servant | 6 | 20.7 |
| Business | 5 | 17.2 |
| Home care | 4 | 13.8 |
| Area council of domicile | ||
| Municipal | 2 | 6.9 |
| Gwagwalada | 21 | 72.4 |
| Kwali | 2 | 6.9 |
| Kuje | 4 | 13.8 |
| Bwari | 2 | 6.9 |
There was a significant association between the age of the patients and their knowledge of FBs (P = 0.009). However, there was no association between sex (P = 0.354), educational status (P = 0.518), occupation (P = 0.167), and area of domicile (P = 0.467) [Table 8].
| Variables | Knowledge | χ2 | P-value | |
|---|---|---|---|---|
| Good | Poor | |||
| n=17 | n=12 | |||
| n(%) | n(%) | |||
| Sex | ||||
| Male | 5 (29.4) | 1 (8.3) | 1.905 | 0.354f |
| Female | 12 (70.6) | 11 (91.7) | ||
| Age group (years) | ||||
| 20–29 | 0 (0.0) | 3 (25.0) | 11.568 | 0.009* |
| 30–39 | 6 (35.3) | 8 (66.7) | ||
| 40–49 | 7 (41.2) | 0 (0.0) | ||
| 50–59 | 4 (23.5) | 1 (8.3) | ||
| Education | ||||
| Secondary | 0 (0.0) | 1 (8.3) | 2.274 | 0.518 |
| Tertiary | 9 (52.9) | 7 (58.3) | ||
| Postgraduate | 7 (41.2) | 4 (33.3) | ||
| Others | 1 (5.9) | 0 (0.0) | ||
| Occupation | ||||
| Home care | 1 (5.9) | 3 (25.0) | 5.060 | 0.167 |
| Civil servant | 11 (64.7) | 3 (25.0) | ||
| Public servant | 3 (17.6) | 3 (25.0) | ||
| Business | 2 (11.8) | 3 (25.0) | ||
| Area council of domicile | ||||
| Municipal | 1 (5.9) | 1 (8.3) | 2.547 | 0.467 |
| Gwagwalada | 14 (82.4) | 7 (58.3) | ||
| Kwali | 1 (5.9) | 1 (8.3) | ||
| Kuje | 1 (5.9) | 3 (25.0) | ||
The test for association between sociodemographic profile and the parents’ attitudes showed a good association between the area of domicile and the attitude (P = 0.003). Still, there was no significant association between age (P = 0.180), gender (P = 0.523), educational status (P = 0.914), and occupation (P = 0.338) [Table 9].
| Variables | Attitudes | χ2 | P-value | |
|---|---|---|---|---|
| Good | Poor | |||
| n=25 | n=4 | |||
| n(%) | n(%) | |||
| Sex | ||||
| Male | 4 (16.0) | 2 (50.0) | 2.429 | 0.180f |
| Female | 21 (84.0) | 2 (50.0) | ||
| Age group (years) | ||||
| 20–29 | 2 (8.0) | 1 (25.0) | 2.248 | 0.523 |
| 30–39 | 12 (48.0) | 2 (50.0) | ||
| 40–49 | 7 (28.0) | 0 (0.0) | ||
| 50–59 | 4 (16.0) | 1 (25.0) | ||
| Education | ||||
| Secondary | 1 (4.0) | 0 (0.0) | 0.521 | 0.914 |
| Tertiary | 14 (56.0) | 2 (50.0) | ||
| Postgraduate | 9 (36.0) | 2 (50.0) | ||
| Others | 1 (4.0) | 0 (0.0) | ||
| Occupation | ||||
| Home care | 4 (16.0) | 0 (0.0) | 3.370 | 0.338 |
| Civil servant | 12 (48.0) | 2 (50.0) | ||
| Public servant | 4 (16.0) | 2 (50.0) | ||
| Business | 5 (20.0) | 0 (0.0) | ||
| Area council of domicile | ||||
| Municipal | 0 (0.0) | 2 (50.0) | 13.782 | 0.003* |
| Gwagwalada | 19 (76.0) | 2 (50.0) | ||
| Kwali | 2 (8.0) | 0 (0.0) | ||
| Kuje | 4 (16.0) | 0 (0.0) | ||
There was no significant association between sex (P = o.633), age group (P = 0.303), education (P = 0.302), occupation (P = 0.736), and area of domicile (P = 0.259) and practices [Table 10].
| Variables | Practices | χ2 | P-value | |
|---|---|---|---|---|
| Good | Poor | |||
| n=19 | n=10 | |||
| n(%) | n(%) | |||
| Sex | ||||
| Male | 3 (15.8) | 3 (30.0) | 0.806 | 0.633f |
| Female | 16 (84.2) | 7 (70.0) | ||
| Age group (years) | ||||
| 20–29 | 3 (15.8) | 0 (0.0) | 3.644 | 0.303 |
| 30–39 | 7 (36.8) | 7 (70.0) | ||
| 40–49 | 5 (26.3) | 2 (20.0) | ||
| 50–59 | 4 (21.1) | 1 (10.0) | ||
| Education | ||||
| Secondary | 0 (0.0) | 1 (10.0) | 3.649 | 0.302 |
| Tertiary | 12 (63.2) | 4 (40.0) | ||
| Postgraduate | 6 (31.6) | 5 (50.0) | ||
| Others | 1 (5.2) | 0 (0.0) | ||
| Occupation | ||||
| Home care | 3 (15.8) | 1 (10.0) | 1.272 | 0.736 |
| Civil servant | 9 (47.3) | 5 (50.0) | ||
| Public servant | 3 (15.8) | 3 (30.0) | ||
| Business | 4 (21.1) | 1 (10.0) | ||
| Area council of domicile | ||||
| Municipal | 1 (5.2) | 1 (10.0) | 4.023 | 0.259 |
| Gwagwalada | 12 (63.2) | 9 (90.0) | ||
| Kwali | 2 (10.5) | 0 (0.0) | ||
| Kuje | 4 (21.1) | 0 (0.0) | ||
χ2 Chi-square test statistic, fFisher’s exact test
DISCUSSION
Children tend to insert foreign materials in the ear, nose, or throat with consequences that may be mild or severe or could even lead to death. Most of the children involved are school age who may encounter these objects in their homes or at school. This makes the role of the parent or teacher vital in preventing, treating, and rehabilitating these children. Most of the respondents (teachers and parents) were in their 4th decade and of the female gender. Furthermore, in both groups, most respondents had a tertiary education and resided in the Gwagwalada area council. Most of the teachers had been teaching for over ten years. For the parents, the majority were civil servants. These show the similarity between the subsets of parents and teachers chosen for this study.
The participant’s knowledge, attitude, and practice were similar, as shown in Figures 1 and 2. They mostly showed good knowledge about FBs, had good attitudes, and demonstrated good practices toward managing a child who had inserted an FB in the ear. This finding is in contrast with findings by other authors.[12] Educating caregivers/parents, teachers, and the general public goes a long way in disaster prevention and management in ENT FB care.[11] People with foreknowledge of how to act in an emergency, like FB insertion, are likely to make the best decisions. Rao et al. published a study in India to evaluate the preparedness of schoolteachers to respond to health emergencies. About 92% of the teachers admitted to not being confident in dealing with emergency health situations.[12] A study in the United States on school nurses to ascertain their preparedness to handle potentially life-threatening emergencies revealed that the majority of the schools did not have an identified personnel who makes important medical decisions on behalf of the students.[13]
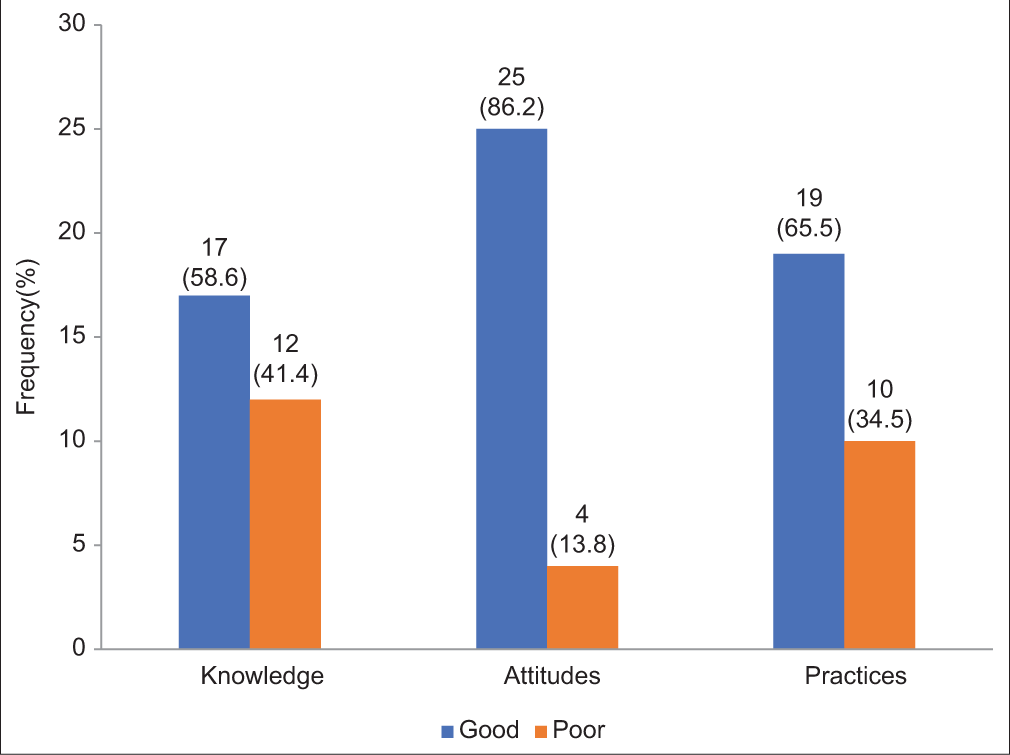
- Knowledge attitude and practices of parents.
Among the teachers, there was a weak association between the gender of the teacher, the age group, level of education, classes being taught, area of domicile of the school, and whether the school was privately owned or government-owned. This shows that the teachers have similar basic ideas of what an FB is and how they can handle it, irrespective of their sociodemographic differences. This may be due to the knowledge they have from their basic training at the colleges of education.
Among the parents, there was a significant positive association between the age group of the parents and their knowledge about FB. This connotes that the older the parent, the more likely they know FBs in ENT. This can be attributed to parental experience. Furthermore, there was a significant association between the area of parents’ domicile and their attitudes. The parents responded from three area councils. The one with the largest population (Gwagwalada) also has the highest number of civil servants with tertiary education. These factors make them more likely to make better decisions in caring for their children as it is likely they have come across such during their school days or have friends or neighbors who are doctors or have some knowledge about FB prevention in ENT. There was a weak association between the other sociodemographic attributes of the parents and the teachers. The number of parents recruited for the study may account for this as they are insufficient to make proper inferences on the association. A study with a larger sample size may need to be conducted to make an appropriate inference.
CONCLUSION
The KAPs of ENT FBs among teachers and parents were generally good. However, in practice, it is observed that children with FB insertions usually present late; thus, there seems to be a disconnect between the knowledge, attitudes, and practices of teachers and parents and what is observed in the hospital. Perhaps, this may be because the study was conducted in the FCT, where the literacy level is higher than in other parts of Nigeria. Hence, there is a need for further studies to be conducted in rural areas where literacy levels are lower, and there is a need for public enlightenment on the dangers of ENT FBs in those areas. This public enlightenment could also target the few teachers and parents with poor KAPs.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
Patient’s consent is not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Ear, nose and throat foreign bodies in Melanesian children: an analysis of 1037 cases. Int J Pediatr Otorhinolaryngol. 2006;70:1539-45.
- [CrossRef] [PubMed] [Google Scholar]
- Foreign bodies in otorhinolaryngology : A study of 128 cases. Int Arch Otorhinolaryngol. 2009;13:394-9.
- [Google Scholar]
- ENT foreign bodies: An experience. Int Arch Otorhinolaryngol. 2018;22:146-51.
- [CrossRef] [PubMed] [Google Scholar]
- Removal of ENT foreign bodies in children. Emerg Med Australas. 2015;27:145-7.
- [CrossRef] [PubMed] [Google Scholar]
- Ear, nose and throat foreign bodies in children: A search for socio-demographic correlates. Int J Pediatr Otorhinolaryngol. 2011;75:510-2.
- [CrossRef] [PubMed] [Google Scholar]
- A review of ear, nose and throat foreign bodies in Sarawak General Hospital. A five year experience. Med J Malaysia. 2012;67:17-20.
- [Google Scholar]
- Foreign body in the ear, nose and throat in children: A five year review in Niger delta. African J Paediatr Surg. 2012;9:3-7.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical spectrum of ear, nose and throat foreign bodies in North Western Nigeria. Afr Health Sci. 2016;16:292.
- [CrossRef] [PubMed] [Google Scholar]
- Childhood nasal foreign bodies: Analysis of 1724 cases. Turk Arch Otorhinolaryngol. 2019;57:187-90.
- [CrossRef] [PubMed] [Google Scholar]
- Management of foreign bodies in the ear, nose and throat in pediatric patients: Real-life experience in a large tertiary hospital. Cureus. 2022;14:e30739.
- [CrossRef] [PubMed] [Google Scholar]
- The importance of education on disasters and emergencies: A review article. J Educ Health Promot. 2019;8:85.
- [CrossRef] [PubMed] [Google Scholar]
- Are schools and teachers prepared to respond to health emergencies in children? A questionnaire study in Mangalore, India. Int J Adv Res. 2014;2:1123-6.
- [Google Scholar]
- The preparedness of schools to respond to emergencies in children: A national survey of school nurses. Pediatrics. 2005;116:e738-45.
- [CrossRef] [PubMed] [Google Scholar]







