Translate this page into:
Gossypiboma – “string of pearls” sign may be diagnostic: A case report

*Corresponding author Clement Odion, Department of Surgery, Irrua Specialist Teaching Hospital, Irrua, Nigeria. clemedz@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Odion C, Okomayin AA, Tagar E, Odigie VI, Okparaojiego CS, Aisabokhale O. Gossypiboma – “string of pearls” sign may be diagnostic: A case report. Ann Med Res Pract 2023;4:3.
Abstract
Gossypiboma is a retained non-absorbable material composed of the common cotton matrix. It is an unexpected surgeon’s “never event” with serious medicolegal implications. We present a case of a young woman who came to our facility 6 days after an emergency cesarean section for prolonged labor in a private hospital with features in keeping with post-operative peritonitis. Pre-operative abdominal radiographs revealed bowel loops that were majorly gasless, except for a row of small round pockets of gas running horizontally across the right hemi-abdomen, giving the “string-of-pearls” sign. She was optimized for an emergency laparotomy. The intraoperative finding was a retained sponge walled off by loops of the dilated small bowel. Within this cavity was found 400 mL of pus. The sponge was removed with ease and the pus was drained with a good post-operative outcome. The finding of a gasless abdomen on a plain radiograph is a thing of concern as small bowel obstruction with or without bowel ischemia is the most feared cause of a gasless abdomen which can be life threatening. Therefore, a gossypiboma should always be considered in a post-surgical patient with abdominal radiographic findings of a gasless abdomen; in particular, with the “string-of-pearls” appearance present. This case highlights that retention of foreign bodies after surgery is a persisting “never event” and as such there is the need to comply with current recommendations on the prevention of retained foreign bodies. The most important approach to reducing the incidence of gossypiboma is prevention. Thus, awareness of this problem is mandatory to avoid unnecessary morbidities.
Keywords
Gossypiboma
Retained sponge
Medicolegal
Foreign body
INTRODUCTION
Gossypiboma is derived from the Latin word “gossypium” meaning “cotton” and the Swahili word “boma” meaning “place of concealment.”[1,2] Thus, gossypiboma is a retained nonabsorbable surgical material composed of the cotton matrix.[2,3] It is an unexpected likely post-operative surgical complication.[4] It is also called “textiloma” because it is made of textile material or “gauzeoma” because it is a foreign body granuloma induced by sponge material.[5] Other synonyms include cottonoid, cottonballoma, and muslinoma.[6] The sponge material can be a piece of gauze, lap pad, towels, gamgee, or an abdominal mop. The first reported case was by Wilson in 1884.[7] Because clinical findings of gossypibomas vary largely, diagnosis can be difficult and as such cause serious morbidity for patients.[4] Most gossypibomas are detected during the first few days after surgery,[8,9] as would be seen from the case report. However, they may remain undetected for many years.[8,9] It can also be asymptomatic.[10] When symptomatic, it can present with obstruction, peritonitis, adhesions, fistula, abscess formation, and erosion into the gastrointestinal tract or even pass through the rectum.[10,11] Transmural migration of an intra-abdominal gossypiboma is rare, though migration into the stomach, colon, bladder, vagina, pericardium, urethra, and diaphragm have been reported.[3,12,13]
The exact incidence of gossypiboma is unknown. This may be due to a general reluctance to publish matters that can have medicolegal implications or because it may initiate widespread critical press coverage.[10,14,15] It was reported that retained surgical items accounted for 1 in 10,000 cases with the majority being surgical sponges.[10] It is commonly found in the abdomen (56%), pelvis (18%), and thorax (11%).[10,16] The risk of gossypiboma is higher in emergency surgeries, prolonged surgeries, operations entailing more than one major procedure, more than one surgical team, failure of surgical or incorrect counts, unexpected intraoperative factors, and high intraoperative blood loss.[15,17-20] Despite awareness, cases of retained surgical sponges abound. Even then, making a pre-operative diagnosis may be challenging. This paper presents a case of post-operative peritonitis, in which plain abdominal radiographs revealed gasless bowel loops and a “string of pearls” sign, thus heightening the suspicion of a retained foreign body.
CASE REPORT
A 25-year-old woman presented to our accident and emergency department with complaints of worsening abdominal pain, abdominal distension, bilious vomiting, and fever following an emergency cesarean section for prolonged labor in a private hospital. She was dehydrated, pale, and febrile (38.7°C). She had unstable vital signs with a pulse rate of 114 beats/min, blood pressure of 90/50 mmHg, and a respiratory rate of 36 cycles. On examination, the abdomen was distended with a midline sub-umbilical incision that gaped at the midportion. There was generalized tenderness with guarding and rebound tenderness. Bowel sounds were hypoactive. She was then optimized and worked up for surgery.
Pre-operative investigations revealed a total white cell count of 8000 cells/mm3, packed cell volume of 27%, and normoelectrolytaemia. Abdominal radiographs revealed a large, well-circumscribed, oval-shaped area of lucency, containing multiple curvilinear lace-like opacities, interspersed with gas, involving predominantly the left hemi-abdomen, and extending just across the lumbar spine. The bowel loops were majorly gasless, except for a row of small round pockets of gas running horizontally across the right hemi-abdomen, giving the string-of-pearls sign, in keeping with small bowel obstruction. There was also complete loss of the abdominal viscera outlines, which includes the liver, spleen, and both renal and psoas muscle shadows, consistent with a featureless abdomen, and suggestive of free intraperitoneal fluid collection. In particular, there was no radiographic evidence of pneumoperitoneum [Figure 1].
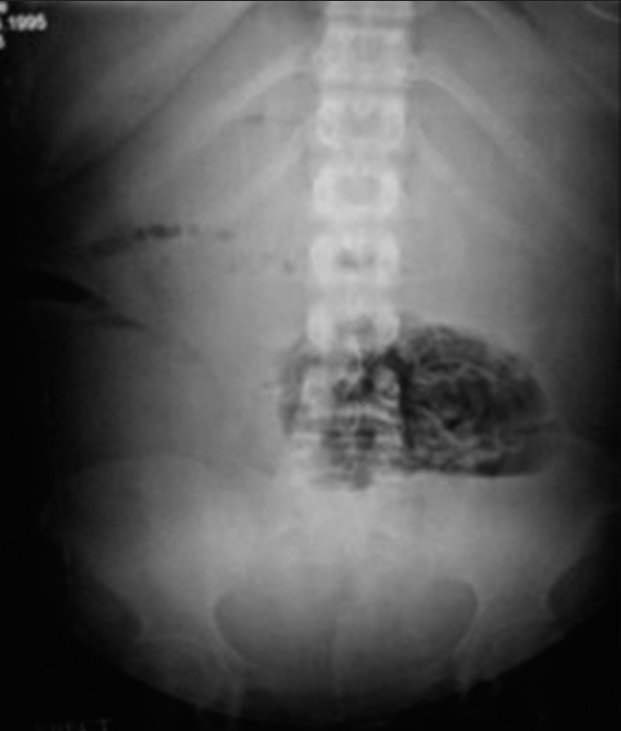
- Erect view of plain abdominal radiograph.
She had an emergency laparotomy and the intraoperative finding was a retained sponge (RS) walled off by loops of dilated small bowel [Figure 2]. Within this cavity was found 400 mL of pus. The pus was drained, and the sponge was retrieved with ease [Figure 3]. The peritoneal cavity was then copiously lavaged and mopped dry.
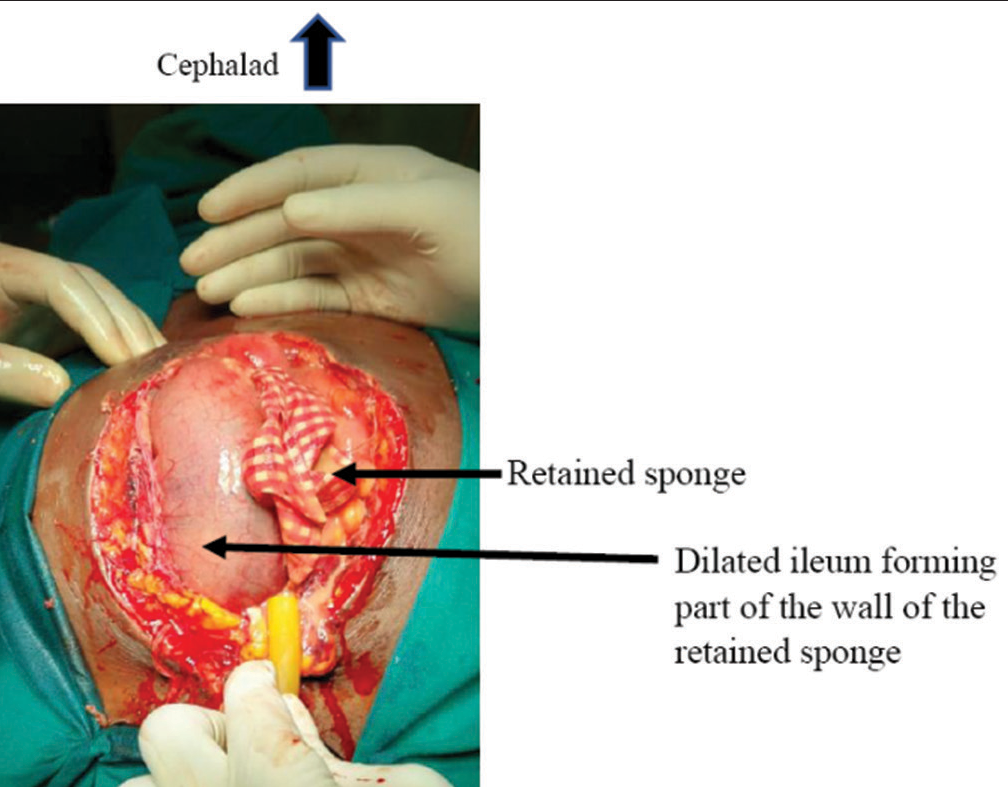
- Intraoperative findings of retained sponge and dilated small bowel.

- Retrieved abdominal mop.
Post-operative recovery was good, and she was discharged 7 days after this surgery in good condition. Follow-up in the clinic has been uneventful.
DISCUSSION
Gossypiboma is mentioned as one of the surgical “never events” in the literature.[10] It is a rare but universal event that is usually underreported for medicolegal reasons.[10] The reported incidence is between 1: 1000 and 1500 abdominal operations.[19,20]
Gossypiboma is most commonly seen in cases of emergency surgery, the unexpected change in the surgical procedure, disorganization (e.g., poor communication), change in the surgical team or scrub nurses, hurried sponge count, long operation time, unstable patients, inexperienced staff, inadequate staff numbers, and obesity.[8,21] In the case presented, it occurred as a complication following an emergency gynecological procedure. Details concerning the composition of the operating team, operation time, and how the swab count was done could not be ascertained.
Although sex is not a risk factor for the occurrence of gossypiboma, it has been reported more in females. This is not unexpected as it has been most frequently reported after gynecological procedures.[14] Apter et al. and Botet del Castillo et al. reported that RS is most frequent after gynecological procedures, followed by upper abdominal surgeries.[22,23] Gawande et al. reported that 63% of their patients with gossypiboma were females, although patient gender was not a risk factor in their study.[15]
The clinical presentation and the time interval between the initial surgery and diagnosis of RS are variable, depending on the location and type of reaction provoked.[14] Two biological reactions are typically triggered: Aseptic fibrinous response and exudative reaction.[8] Most commonly, aseptic fibrinous inflammatory reactions and adhesions encapsulate the RS in the omentum and nearby organs.[14] Thus, diagnosis is difficult as a result of the less severe symptoms and the delay in onset from previous surgery.[14] Patients usually remain asymptomatic, and the RSs are detected incidentally, or they present with pseudotumor.[14] This was the case with the report by Agbonrofo et al., where the patient had presented with a lower abdominal mass with computed tomography (CT) scan considerations of (1) calcified mesenteric cyst and (2) calcified hydatid cyst.[6]
The other type of biological response, the exudative inflammatory reaction, presents with an abscess or chronic internal or external fistula formation.[14] The resultant abscess may lead to an external opening (a discharging sinus) or open into an adjacent hollow organ such as the stomach, intestine, bladder, or vagina.[14] This usually presents much earlier than the fibrinous reaction.[14] This was the case with our patient, who had presented 6 days after an emergency cesarean section in a private facility with the intraoperative finding of a retained mop that was surrounded by 400 mL of pus.
Internal extrusion of RS has been reported to occur in all parts of the intestinal tract, with the most frequent sites being the ileum and colon.[14] The erosion process may take years and within this period, most patients are symptomatic and present with abdominal pain, nausea, vomiting, anemia, diarrhea, malnutrition, and weight loss.[14] Spontaneous expulsion of the RS through the rectum after a variable period of 10 days to 15 years has also been reported, largely due to the peristaltic activity of the intestines in propelling the foreign body.[14] Manabe et al. reported a case of spontaneous expulsion of RS through the rectum.[24] Crossen and Crossen reported 37 cases in which the sponges were passed through the rectum, 24 were found within the bowel at surgery, and ten cases in which the sponges were found in the process of penetrating the bowel wall.[25]
Although radiological investigations are quite sensitive in picking up gossypibomas, they are limited in scope especially if the sponge does not have any radiological marker on itself.[8] This is because the cotton material can simulate hematomas, granulomas, abscess cavities, cystic masses, or neoplasms.[8,21] Even then, the markers may be distorted by folding, twisting, or disintegration over time.[14] Thus, even with the presence of a radio-opaque marker, RS can be difficult to visualize and may be overlooked or an erroneous diagnosis made.[14] In one study involving ten patients with RS, all the swabs had radio-opaque markers, but the diagnosis was made by plain X-ray in only four patients, supplemented by CT or ultrasound scan in two of these.[14] In the case presented here, a plain X-ray revealed a gasless abdomen with a “string of pearls” sign, thus heightening the suspicion of a retained foreign body. On erect or decubitus radiographs, small pockets of gas may be seen trapped between the valvulae conniventes, creating multiple tiny air-fluid levels that give the appearance of “string-of-pearls.”[26] The finding of a gasless abdomen on a plain radiograph is a thing of concern as small bowel obstruction with or without bowel ischemia is the most feared cause of a gasless abdomen which can be life-threatening.[27] Therefore, a gossypiboma should always be considered in a post-surgical patient with abdominal radiographic findings of a gasless abdomen; in particular, with the “string-of-pearls” appearance present. By contrast, CT should be preferred for a definitive diagnosis.[4] CT usually reveals a rounded mass with a dense central part and an enhancing wall or gas bubbles or calcific depositions.[4] On magnetic resonance imaging, gossypibomas may appear as low signal intensity lesions on T2-weighted images with wavy, striped, or spotted appearances.[4,28]
Once a diagnosis of gossypiboma is made, treatment is surgical retrieval of the sponge. Most times, the diagnosis is intraoperative as the case presented. Sometimes, the sponge may not be visible directly, because surgical tampons can be surrounded by omentum and bowel.[4] Open surgery is a common approach; however, depending on the location, size of the foreign body, and skill of the operator, minimally invasive techniques such as endoscopy or laparoscopy have proven effective.[2,3] In cases where transmural migration is suspected, endoscopic treatments are mostly unsuccessful.[3] In addition to retrieval of the sponges, surgical interventions may include drainage of abscess, bowel resection and anastomosis, creation of stomas, adhesiolysis, etc., depending on the presentation.
Gossypiboma is an unexpected surgical outcome. However, it can be prevented. Thus, a systematic approach is essential to reduce its incidence.[10] Many techniques are available to prevent this problem. Instrument and swab counts should be performed at various stages during surgery. This includes count performed before the commencement of any procedure, at the time of addition of a new item, before the closure of a cavity, at the time of closure of fascia and at skin closure, or even during a change of scrub nurses. If any discrepancy is found, the entire surgical team should look for the item.[10] This is especially important in obese patients and emergency surgeries.[14] A simple and effective surgical safety protocol like the World Health Organization checklist can also be used as part of institutional policies aimed at improving surgical safety and patient care.[10] Where possible sponges tagged with radio-opaque markers should be used.[3] If there are concerns over a retained surgical swab, the use of intra- or post-operative radiography to assist in confirming the suspicion would be indicated.[3,27] This is enabled by the aforementioned “tagging” of modern surgical swabs and sponges, which will appear as hypodense linear structures on plain radiographs if retained.[3,29] Other measures include attaching a forceps to any pack before using it in the abdominal cavity, using swabs on the stick rather than free swabs once in the body cavity, and avoiding the use of untrained nursing personnel and unnecessary hurry during surgery.[5] Newer technologies are being developed to decrease the incidence of gossypibomas like radiofrequency chip identification by barcode scanner.[20,30]
CONCLUSION
This report presents an early manifestation of gossypiboma, highlighting its occurrence usually following emergency and gynecological procedures. It is a rare, but avoidable postoperative surgical complication. It is usually asymptomatic and generally has non-specific radiologic findings. Clinical presentation is extremely variable, with presentation after 40 years being reported.[17] The finding of a gasless abdomen on a plain radiograph is a thing of concern as small bowel obstruction with or without bowel ischemia is the most feared cause of a gasless abdomen which can be life-threatening. Therefore, a gossypiboma should always be considered in a post-surgical patient with abdominal radiographic findings of a gasless abdomen; in particular, with the “string-of-pearls” appearance present. It should not be dismissed as a “never event.” Thus, awareness of this problem is mandatory to avoid unnecessary morbidities. Therefore, surgeons should comply with current recommendations on the prevention of retained foreign bodies, including the use of radiological markers and routine pre- and post-operative sponge count.[8] Although human errors cannot be completely eliminated, continuous medical training and strict adherence to regulations should reduce the incidence to a minimum.[14]
Declaration of patient consent
Patient’s consent not required as patient’s identity was not disclosed nor compromised.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Diagnostic challenges in patients with tumours: Case 1. Gossypiboma (foreign body) manifesting 30 years after laparotomy. J Clin Oncol. 2003;21:3700-1.
- [CrossRef] [PubMed] [Google Scholar]
- Asymptomatic gossypiboma mimicking a liver mass. Turk J Surg. 2010;26:225-8.
- [CrossRef] [Google Scholar]
- Presentation and surgical management of a gossypiboma presenting with small bowel obstruction. Clin J Gastroenterol. 2021;14:1067-70.
- [CrossRef] [PubMed] [Google Scholar]
- A case of intestinal obstruction caused by gossypiboma recognized 9 years later. Turk J Colorectal Dis. 2021;31:163-6.
- [CrossRef] [Google Scholar]
- Gossypiboma or textiloma: A report of 2 cases and strategies for prevention. Am J Med Case Rep. 2014;2:123-5.
- [Google Scholar]
- Gossypiboma masquerading as calcified mesenteric cyst: A case report. W J Biomed Res. 2021;8:56-60.
- [Google Scholar]
- Foreign bodies left in the abdomen after laparotomy. Trans Am Gynecol Soc. 1884;9:109-12.
- [Google Scholar]
- Gossypiboma posing as a diagnostic dilemma: A case report and review of the literature. Case Rep Surg. 2014;2014:713428.
- [CrossRef] [PubMed] [Google Scholar]
- Small bowel perforation due to gossypiboma caused acute abdomen. Case Rep Surg. 2013;2013:219354.
- [CrossRef] [PubMed] [Google Scholar]
- Gossypiboma: A case series and literature review. Ethiop J Health Sci. 2020;30:147-9.
- [CrossRef] [Google Scholar]
- Improving safety in the operating room: A systematic literature review of retained surgical sponges. Curr Opin Anesthesiol. 2009;22:207-14.
- [CrossRef] [PubMed] [Google Scholar]
- Transgastric migration of retained intraabdominal surgical sponge: Gossypiboma in the bulbus. Intern Med. 2008;47:613-5.
- [CrossRef] [PubMed] [Google Scholar]
- Transmural migration of retained surgical sponges: A systematic review. Obstet Gynecol Surv. 2008;63:465-71.
- [CrossRef] [PubMed] [Google Scholar]
- Retained surgical sponges (gossypiboma) Asian J Surg. 2005;28:109-15.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for retained instruments and sponges after surgery. N Engl J Med. 2003;348:229-35.
- [CrossRef] [PubMed] [Google Scholar]
- Wrong-site surgery, retained surgical items, and surgical fires: A systematic review of surgical never events. JAMA Surg. 2015;150:796-805.
- [CrossRef] [PubMed] [Google Scholar]
- Gossypiboma of the abdomen and pelvis; a recurring error. Ann Afr Surg. 2017;14:44-7.
- [CrossRef] [Google Scholar]
- Risk factors for retained surgical foreign bodies: A meta-analysis. OPUS. 2009;12:21-7.
- [Google Scholar]
- Risk factors for retained surgical items: A meta-analysis and proposed risk stratification system. J Surg Res. 2014;190:429-36.
- [CrossRef] [PubMed] [Google Scholar]
- Retained foreign bodies after surgery. J Surg Res. 2007;138:170-4.
- [CrossRef] [PubMed] [Google Scholar]
- Gossypiboma, a rare cause of acute abdomen: A case report and review of literature. Int J Crit Illn Inj Sci. 2011;1:157-60.
- [CrossRef] [PubMed] [Google Scholar]
- Gossypiboma in the early postoperative period: A diagnostic problem. Clin Radio. 1990;42:128-9.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of retained abdominal gauze swabs. Br Surg. 1995;82:227-8.
- [CrossRef] [PubMed] [Google Scholar]
- A case of retained surgical sponge penetrated into the sigmoid colon. Nippon Igaku Hoshasen Gakkai Zasshi. 1997;57:279-80. [In Japanese]
- [Google Scholar]
- Foreign Bodies Left in the Abdomen: The Surgical Problems, Cases, Treatment, Prevention In: The Legal Problems, Cases, Decisions, Responsibilities. St. Louis: C.V. Mosby Co.; 1940. p. :704-37.
- [Google Scholar]
- Imaging modalities for evaluation of intestinal obstruction. Clin Colon Rectal Surg. 2021;34:205-18.
- [CrossRef] [PubMed] [Google Scholar]
- Gasless abdomen in the adult: What does it mean? AJR Am J Roentgenol. 2008;191:1093-9.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of gossypibomas: Pictorial review. AJR Am J Roentgenol. 2009;193(6 Suppl):S94-101.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of retained surgical items: A pictorial review including new innovations. Indian J Radiol Imaging. 2017;27:354-61.
- [Google Scholar]
- Initial clinical evaluation of a handheld device for detecting retained surgical gauze sponges using radiofrequency identification technology. Arch Surg. 2006;141:659-62.
- [CrossRef] [PubMed] [Google Scholar]






