Translate this page into:
Any correlation between severity of symptoms and the adenoid nasopharyngeal ratio?

*Corresponding author Enoch Auta Dahilo, Department of Otorhinolaryngology, Head and Neck Surgery, University of Abuja/University of Abuja Teaching Hospital, Gwagwalada, Nigeria. edahiloa@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Dahilo EA, Itanyi UD, Yikawe SS, Folorunso DF, Ibekwe TS. Any correlation between severity of symptoms and the adenoid nasopharyngeal ratio? Ann Med Res Pract 2023;4:2.
Abstract
Objective:
Adenoid Hypertrophy is a common childhood condition that presents with mouth breathing, nasal discharge, snoring and sleep apnea. Lateral Nasopharyngeal X-ray aids diagnosis and assessment of patency of the Nasopharyngeal air column through Adenoid Nasopharyngeal Ratio (ANR). This study aims to correlate ANR with symptoms and signs of Adenoid Hypertrophy.
Material and Methods:
A retrospective study conducted in the Ear, Nose and Throat/Head and Neck Surgery (ENT/HNS) Department of University of Abuja Teaching Hospital, Gwagwalada from January 2019 to December 2021. The case notes and Lateral Nasopharyngeal X-rays of 66 Children aged between 2months to 11 years, with suspected Adenoid Hypertrophy were retrieved and relevant retrieved data analyzed.
Results:
A total of 66 patients were enrolled into this study with 50 (75.76%) males and 16 (24.24%) females. The age range was between 2 months to 11 years, with a mean of 3.65±2.76 years. ANR ranged from 0.03 to 0.94 with mean 0.71±0.15. Out of the 66 participants, 30 (46.15%) had ANR of 0.7, while 35 (53.85%) had ANR of > 0.7. Linear regression analysis showed association between age and ANR (P < 0.05). Snoring was the most common symptom (92.42%), followed by Mouth breathing (89.39%) and Nasal Discharge (77.27%). Majority of patients (88.6%) had a Mild Symptom Score. There was no statistically significant relationship between any of the clinical features and ANR.
Conclusion:
There is no significant correlation between the clinical features and adenoid nasopharyngeal ratio.
Keywords
Adenoids
Adenoid-nasopharyngeal ratio
Lateral nasopharyngeal X-ray
INTRODUCTION
The nasopharyngeal tonsils (Adenoids) are part of the waldeyer’s ring of lymphoid tissue that protects the airway from inhaled pathogens.[1] They are located at the junction of the roof and the posterior wall of the nasopharynx, behind the posterior choana.[1,2] They are also closely related to the opening of the eustachian tube, and if enlarged can block the pharyngeal opening of this tube.[1,3] In the early childhood, their immunologic functions are more elaborate; they produce immunoglobulins that help to prevent pathogenic organisms from getting into the aerodigestive tract.[2] However, with repeated exposure to infective agents, allergens, and other triggers, adenoids become enlarged and eventually lose or have significant reductions in their immunologic capabilities.[4-7] Enlarged adenoids cause symptoms mainly through obstructive effects in the nasopharynx. Obstruction or narrowing of the nasopharyngeal air column will cause nasal obstruction, mouth breathing, and snoring.[2,8] Significant levels of obstructions can cause brief periods of apnea during sleep that will necessitate the child to wake up to “catch his/her breath.”[9,10] Blockage of the pharyngeal opening of THE Eustachian tube may present with features suggestive of otitis media, and otitis media with effusion (OME).[1,3,11] However, symptoms of adenoid hypertrophy (AH) could also occur in situations where the adenoid (even when not significantly enlarged) serves as a reservoir of infection in the pharynx. This can lead to infective sequelae such as acute otitis media and/or chronic rhinosinusitis (in childhood).[5,11]
Due to its location, adenoid cannot be easily examined by nonEar, Nose, and Throat (ENT) Surgeons, because this usually requires endoscopic examination or mirror examination in cooperative children where endoscopy is not readily available.[12] However, other examination findings, such as reduced nasal patency, nasal discharge, and noisy breathing can be picked. Features of adenoid facies such as pinched nose, short upper lip, open mouth posture, elongated face, prominent upper teeth, and high arched palate may be observed in longstanding cases.[10,13,14] Examination of a child suspected of having AH should also aim to rule out other possible causes of nasal obstruction such as enlarged inferior turbinates, nasal polyps, deviated nasal septum, and juvenile masses in older children[2,15,16] The size of the tonsils should always be checked and documented, as a coexisting tonsillar disease is common among these patients. Obstructive sleep apnea in the long run can affect the heart and the lung.[17-19] Psychosocial problems such as learning disabilities, daytime sleepiness, bed wetting, and social isolation could occur in some patients.
AH is a common childhood condition that is being diagnosed by various specialists such as pediatricians and otorhinolaryngologists. The widely accepted goal standard for diagnosis of AH is endoscopic evaluation of the nasopharynx.[7,20,21] Other methods of diagnosis are as follows: clinical assessment, lateral nasopharyngeal X-ray, rhinomanometry, nasal rhinometry, magnetic resonance imaging (MRI), and computed tomography (CT) scan.[7,16,20-22] Endoscopic assessment, though reliable, is invasive and difficult to perform in younger children (who are more frequently affected).[11,23,24] MRI in younger children has similar challenges of being difficult to perform and often associated with motion artifacts. Furthermore, investigations such as CT scans, MRI, nasal rhinometry, rhinomanometry, and nasal endoscopy are not readily available in resource-constrained settings such as ours. This leaves lateral nasopharyngeal X-ray (LNX) as the most suitable investigative tool. In addition, LNX is non-invasive, cheap, and easy to perform and familiar to many physicians and surgeons.
LNX evaluates the patency of the nasopharyngeal airway, by comparing the size of the adenoid tissue with the nasopharyngeal space.[25,26] In susceptible children in early childhood, the adenoid tissue grows at a faster rate than the nasopharynx; this causes the narrowing of the nasopharyngeal air column, making symptoms worse in children below the age of 5 years.[2,3,22] As the child grows older, the nasopharynx increases in size relative to the adenoid, thus creating more space in the nasopharynx, and in most children causing relief of symptoms in later childhood. The drawbacks of LNX are the likelihood of bias in interpretation of the images obtained. Several authors have made attempts to standardize the findings obtained from LNX and to correlate such findings with endoscopic features.[25-27] Fujioka et al. have the first to introduce the concept of adenoid nasopharyngeal ratio (ANR), in 1979 as a way to objectively assess the patency of the nasopharyngeal air column in patients with AH.[25] They considered an ANR of 0.8 to be indicative of enlarged adenoids.[25] ANR is taken as the ratio between the distance measured from the maximal convexity of the adenoid to the anterior margin of the basiocciput (adenoid thickness) and the distance along a line from the posterior edge of the hard palate to the spheno-occipital synchondrosis on the base of the skull.[25,26] This study aims to correlate ANR with symptoms and signs of AH.
MATERIAL AND METHODS
This was a retrospective study conducted in the ENT/HN Department of the University of Abuja Teaching Hospital, Gwagwalada from January 2019 to December 2021. The case notes and lateral nasopharyngeal X-rays of 103 children aged between 2 months and 15 years, that were diagnosed with AH were retrieved and relevant information such as demographics, symptoms, and examination findings were extracted. Out of the 103 participants, only 66 had their information complete. Symptoms assessed include; mouth breathing, snoring, sleep apnea, hearing loss, dyspnea, daytime sleepiness, and failure to thieve. Other symptoms evaluated include a history of ear discharge, nasal discharge, refusal of feeds, voice change, and cough. A symptomatology score (SS) was used to grade the severity of the patient’s symptoms. All symptoms were assigned the following numeric values; 0-No (symptom is absent) and 1 – Yes (symptom is present). A patient could obtain a maximum SS of 14. This was classified as; mild (1–5), moderate (6–10), and severe (11–14).[26] Examination findings were also extracted from the case file. Findings such as tympanic membrane appearance, external nasal appearance, nasal patency, nasal septal appearance, inferior turbinate condition, presence of nasal mass, tonsillar size, presence of tonsillar exudates, uvula, and appearance of the posterior pharyngeal wall.
Lateral pharyngeal X-ray images of participants were analyzed. ANR was calculated by dividing the adenoid measurement by the nasopharyngeal measurement. The adenoid measurement (CE) corresponded to the distance from the point of maximal convexity of the adenoid shadow to a line along the anterior margin of the basiocciput. The nasopharyngeal measurement (CD) corresponded to the distance between the posterior border of the hard palate and the anteroinferior edge of the spheno-basioccipital synchondrosis [Figure 1]. When the synchondrosis could not be clearly visualized, this was substituted with a point on the anterior edge of the basiocciput which is closest to the intersection of a perpendicular line drawn from the convexity of the adenoid tissue, and a line along the anterior margin of the basiocciput (Elwany’s modification of Fujioka’s method).[26]

- Lateral PNS X-ray, AB: Line along anterior margin of basiocciput, C: Sphenobasioccipital synchondrosis, CD: Nasopharynx, CE: Adenoidal tissue.
Data were entered into an excel spreadsheet. Data were presented in simple descriptive forms as proportions using tables and chats. Means and frequencies were calculated. The relationship between categorical variables was compared using fisher’s exact test. Regression analysis was used to compare ANR with the age of participants, and ANR with the clinical features of participants. ANR of ≤0.7 was considered as normal and an ANR of >0.7 was considered as enlarged in this study.[26] The level of significance for this study was set at 0.05.
RESULTS
A total of 66 patients were enrolled in this study. Out of these, 50 (75.76%) were male and 16 (24.24%) were female. The mean age was 3.65 ± 2.76 years, with ages ranging from 2 months to 15 years. Median and modal ages were 3 years [Table 1].
| Variables | Frequency (%) n=66 |
|---|---|
| Age group (Years) | |
| 0–3 | 39 (59.10) |
| 4–6 | 20 (30.30) |
| 7–9 | 3 (4.50) |
| 10–12 | 3 (4.50) |
| 13–15 | 1 (1.60) |
| Sex | |
| Males | 50 (75.76) |
| Females | 16 (24.24) |
The mean ANR was 0.71 ± 0.15. The median ANR was 0.73, while the modal ANR was 0.75. ANR ranged from 0.03 to 0.94. Out of the 35 participants, 30 (46.15%) had an ANR of ≤0.7, while 35 (53.85%) had an ANR of >0.7 [Figure 2]. Linear regression analysis showed an association between age and ANR (P = 0.003, R2 = 0.13).
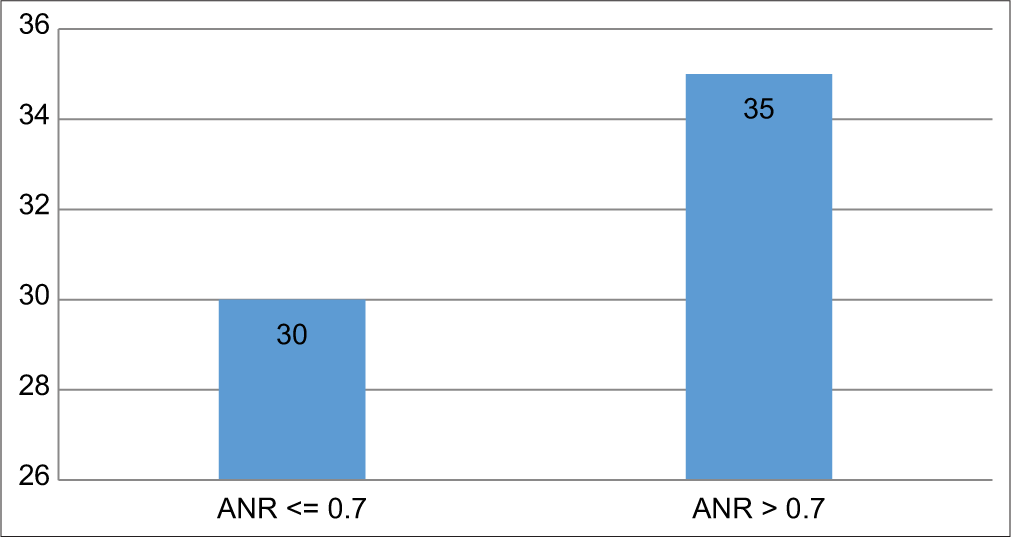
- Adenoid nasopharyngeal ratio among participants.
Snoring was the most common symptom (92.42%), followed by mouth breathing (89.39%) and nasal discharge (77.27%). Details are in [Table 2]. The majority of patients (88.6%) had a mild symptom score [Table 3]. Examination findings revealed that, 54 (81.82%) participants had adequate nasal patency, while 2 (3.03%) had obstructed nasal cavities on examination. Majority of patients (44.52%) had grade 3 tonsillar enlargements [Table 4].
| Symptoms | Frequency (%) n=66 |
|---|---|
| Ear discharge | 3 (4.55) |
| Nasal discharge | 51 (77.27) |
| Sneezing bouts | 11 (16.67) |
| Nose bleeds | 2 (3.03) |
| Refusal of feeds | 2 (3.03) |
| Voice change | 2 (3.03) |
| Cough | 14 (21.21) |
| Mouth breathing | 59 (89.39) |
| Snoring | 61 (92.42) |
| Sleep apnea | 40 (60.61) |
| Hearing loss | 2 (3.03) |
| Dyspnea | 10 (15.15) |
| Daytime sleepiness | 5 (7.58) |
| Failure to thrive | 1 (1.52) |
| Symptom score | Proportion (%) n=66 |
|---|---|
| Mild (symptom score of 1–5) | 88.60 |
| Moderate (symptom score of 6–10) | 11.40 |
| Clinical findings | Frequency (%) n=66 |
|---|---|
| Tympanic membrane (right) | |
| Normal | 62 (93.94) |
| Dull | 2 (3.03) |
| Retracted | 1 (1.52) |
| Wax Impaction | 1 (1.52) |
| Tympanic membrane (Left) | |
| Normal | 63 (95.45) |
| Dull | 2 (3.03) |
| Wax impaction | 1 (1.52) |
| External nasal examination | |
| Normal | 65 (98.48) |
| Deformed | 1 (1.52) |
| Nasal patency | |
| Adequate | 54 (81.82) |
| Reduced | 10 (15.15) |
| Obstructed | 2 (3.03) |
| Nasal Septum | |
| Central | 66 (100) |
| Turbinate | |
| Normal | 51 (77.27) |
| Enlarged | 15 (22.73) |
| Tonsil size | |
| Grade 1 | 10 (6.45) |
| Grade 2 | 56 (36.13) |
| Grade 3 | 69 (44.52) |
| Grade 4 | 20 (12.90) |
| Uvula | |
| Normal | 66 (100) |
| Posterior pharyngeal wall | |
| Normal | 63 (95.45) |
| Granular | 3 (4.55) |
| Stridor | |
| Yes | 1 (1.52) |
| No | 65 (98.48) |
There was no statistically significant relationship between any of the clinical features and ANR (P > 0.05) [Table 5].
| Clinical features | ANR | |
|---|---|---|
| ANR ≤0.7 | ANR >0.7 | |
| Ear discharge | ||
| No | 31 | 32 |
| Yes | 0 | 3 |
| (Fe χ2), P=0.09 | ||
| Nasal discharge | ||
| No | 6 | 9 |
| Yes | 25 | 26 |
| (χ2), P=0.538 | ||
| Mouth Breathing | ||
| No | 3 | 4 |
| Yes | 28 | 31 |
| (Fe χ2), P=0.818 | ||
| Snoring | ||
| No | 4 | 1 |
| Yes | 27 | 34 |
| (Fe χ2), P=0.124 | ||
| Sleep apnea | ||
| No | 14 | 12 |
| Yes | 17 | 23 |
| (χ2),P=0.367 | ||
| Hearing loss | ||
| No | 29 | 35 |
| Yes | 2 | 0 |
| (Fe χ2), P=0.127 | ||
ANR: Adenoid nasopharyngeal ratio
DISCUSSION
AH is a common childhood disease that is often neglected by caregivers and misdiagnosed by primary care medical practitioners. If left untreated, it may lead to unwanted pathological changes in the heart, lungs, and craniofacial growth of a child.[10,13,14,17-19,28] This study assessed the ANR of participants and compared it with the clinical features that they presented. A total of 66 participants were enrolled in this study. Out of these, 50 (75.76%) were male and 16 (24.24%) were female. This finding is in agreement with most studies conducted on AH.[11,12,21,25-27,29-33] However, Feres et al.,[32] in a cross-sectional study on the reliability of adenoid evaluation among 40 participants, reported equal sex distribution. The mean age of participants in the study was 3.65 ± 2.76 years (2 months–15 years). The age group 0–3 years was the most commonly observed (59.10%) age group in this study. Similar findings were reported by Adedeji et al.[30] who conducted a hospital-based cross-sectional study on the correlation of ANR and symptoms among 90 participants. They reported a mean age of 3.0 ± 2.3 years.
The most common symptoms observed in this study were; snoring (92.42%), mouth breathing (89.39%), and nasal discharge (77.27%). There is no universally agreed symptom score classification system for AH. In this study, for the symptom score (SS), we categorized participants into; those with mild (symptom score of 1–5), moderate (symptom score of 6–10), and severe symptoms (symptom score of 11–15).[26] We had 88.6% of participants who had mild symptoms and 11.4% of participants who had moderate symptoms. We did not have any participant who had severe symptoms in this study. Furthermore, we did not observe any relationship between ANR and the clinical features of the participants. This was corroborated by the study conducted by Hamza and Ranjith, on 100 children in a government hospital in India.[12] They reported snoring and mouth breathing in 75 participants.[12] A cross-sectional study conducted among 90 children in Usmanu Danfodiyo University Teaching Hospital observed that all the participants presented with snoring, mouth breathing and recurrent upper airway infection.[29] Adedeji et al.[30] reported similar findings of nasal obstruction, mouth breathing, snoring, and nasal discharge in a hospital-based study in Southwest Nigeria with a statistically significant association between ANR and age, similar to the index study. However, in variance to our findings, Rilwanu et al.[29] and Adedeji et al.[30] reported an association between ANR and symptoms of AH.[29,30] Other studies also found an association between ANR and symptoms.[21,26,31] Although Kolo et al.[33] reported 38.5% having snoring and mouth breathing 35.9%; findings which are at variance with our observations on clinical features, their study also did not observe any statistically significant association between ANR. Both studies had sample sizes that were <40. This may have been responsible for the poor association between ANR and symptoms. However, these findings may need to be further investigated to re-evaluate the importance of ANR in contemporary ENT practice in the 21st century.
With advances in pediatric endoscopy, attention should be shifted toward endoscopic evaluation of AH in patients being considered for adenoid surgery. A study conducted in the Department of Otorhinolaryngology of Baskent University, Ankara Turkey observed that ANR correlated with endoscopic findings.[21] In another study that compared adenoid size in lateral radiographic, pathologic, and endoscopic measurements in 27 children with OME, they reported a mean ANR of 7.81 ± 2.52.[11] Since these authors studied patients with AH and OME, it is likely that these patients already had severe disease, and this predisposed them to have OME, thereby very likely accounting for the higher values of ANR in their participants.
The advantage of endoscopic evaluation and subsequent reduction in the need for repeated radiation exposure in children cannot be over-emphasized.
CONCLUSION
Common symptoms of AH are snoring, mouth breathing, nasal discharge, and sleep apnea. ANR is an objective method to access the obstruction in the nasopharyngeal air column caused by AH, using lateral nasopharyngeal X-ray. Majority of the participants presented with snoring, mouth breathing, and sleep apnea. There was an association between ANR and the age of participants (P = 0.0007), but no statistically significant relationship between ANR and clinical features of AH.
Declaration of patient consent
Patient consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Anatomy and physiology of the palatine tonsils, adenoids, and lingual tonsils. World J Otorhinolaryngol Head Neck Surg. 2021;7:155-60.
- [CrossRef] [PubMed] [Google Scholar]
- Adenoids in children: Advances in immunology, diagnosis, and surgery. Clin Anat. 2014;27:346-52.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomy, Head and Neck, Nasopharynx Treasure Island (FL): StatPearls Publishing; 2021.
- [Google Scholar]
- The role of the adenoids in pediatric chronic rhinosinusitis. Med Sci. 2019;7:35.
- [CrossRef] [PubMed] [Google Scholar]
- Sinus and adenoid inflammation in children with chronic rhinosinusitis and asthma. Ann Allergy Asthma Immunol. 2015;114:103-10.
- [CrossRef] [PubMed] [Google Scholar]
- Adenoid hypertrophy in children with allergic disease and influential factors. Int J Pediatr Otorhinolaryngol. 2015;79:694-7.
- [CrossRef] [PubMed] [Google Scholar]
- The accuracy of diagnostic tests for adenoid hypertrophy. J Am Dent Assoc. 2014;145:247-54.
- [CrossRef] [PubMed] [Google Scholar]
- Diseases of the adenoids and tonsils in children. Surgery (Oxford). 2021;39:617-24.
- [CrossRef] [Google Scholar]
- Persistent adenoids and their secondary effects. Int J Otorhinolaryngol Head Neck Surg. 2020;6:1245-9.
- [CrossRef] [Google Scholar]
- The effect of adenoid hypertrophy on maxillofacial development: An objective photographic analysis. J Otolaryngol Head Neck Surg. 2016;45:48.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of adenoid size in lateral radiographic, pathologic, and endoscopic measurements. Electron Physician. 2018;10:6935-41.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of size of adenoid-comparison of adenoidal nasopharyngeal ratio and nasal endoscopy in children with chronic adenoiditis. Int J Res Med Sci. 2019;7:776-81.
- [CrossRef] [Google Scholar]
- Surgical-orthodontic management of bilateral multiple impactions in non-syndromic patient. BMJ Case Rep. 2013;2013:bcr2012007748.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of adenoidal obstruction in children: Clinical signs versus roentgenographic findings. Pediatrics. 1999;104(Supplement_2):370.
- [CrossRef] [Google Scholar]
- Assessment of adenoidal obstruction in children: Clinical signs versus roentgenographic findings. Pediatrics. 1998;101:979-86.
- [CrossRef] [PubMed] [Google Scholar]
- Obstructive sleep apnea syndrome: Links betwen pathophysiology and cardiovascular complications. Clin Invest Med. 2015;38:362-70.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiovascular complications in obstructive sleep apnea syndrome. Multidiscip Cardio Annal. 2019;10:e91534.
- [CrossRef] [Google Scholar]
- Treatment options for pediatric obstructive sleep apnea. Curr Probl Pediatr Adolesc Health Care. 2016;46:27-33.
- [CrossRef] [PubMed] [Google Scholar]
- The role of rhinomanometry after nasal decongestant test in the assessment of adenoid hypertrophy in children. Int J Pediatr Otorhinolaryngol. 2012;76:352-6.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation between adenoid-nasopharynx ratio and endoscopic examination of adenoid hypertrophy: A blind, prospective clinical study. Int J Pediatr Otorhinolaryngol. 2009;73:1532-5.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of adenoid hypertrophy: A systematic review and meta-analysis. Sleep Med Rev. 2018;38:101-12.
- [CrossRef] [PubMed] [Google Scholar]
- ACE grading-a proposed endoscopic grading system for adenoids and its clinical correlation. Int J Pediatr Otorhinolaryngol. 2016;83:155-9.
- [CrossRef] [PubMed] [Google Scholar]
- Adenoids: Comparison of radiological assessment methods with clinical and endoscopic findings. J Laryngol Otol. 1992;106:342-4.
- [CrossRef] [PubMed] [Google Scholar]
- Radiographic evaluation of adenoidal size in children: Adenoidal-nasopharyngeal ratio. Am J Roentgenol. 1979;133:401-4.
- [CrossRef] [PubMed] [Google Scholar]
- The adenoidal-nasopharyngeal ratio (AN ratio) J Laryngol Otol. 1987;101:569-73.
- [CrossRef] [PubMed] [Google Scholar]
- Radiographic adenoid evaluation-suggestion of referral parameters. J Pediatr. 2014;90:279-85.
- [CrossRef] [PubMed] [Google Scholar]
- Association between adenoid-nasopharyngeal ratio and tympanogram width in adenoid hypertrophy patients. Asian J Oncol. 2021;8:42-6.
- [CrossRef] [Google Scholar]
- Correlation between radiographic adenoidnasopharyngeal ratio and clinical symptoms of adenoid hypertrophy in a tertiary health institution in North West Nigeria. Asian J Med Sci. 2022;13:161-6.
- [CrossRef] [Google Scholar]
- Correlation between adenoidal nasopharyngeal ratio and symptoms of enlarged adenoids in children with adenoidal hypertrophy. Afr J Paediatr Surg. 2016;13:14-9.
- [CrossRef] [PubMed] [Google Scholar]
- Role of adenoid-nasopharyngeal ratio in assessing adenoid hypertrophy. Indian J Otolaryngol Head Neck Surg. 2018;71(Suppl 1):469-73.
- [CrossRef] [PubMed] [Google Scholar]
- Reliability of radiograpjic parameters in adenoid evaluation. Braz J Otorhinolaryngol. 2012;78:80-90.
- [CrossRef] [PubMed] [Google Scholar]
- Plain radiographic evaluation of children with obstructive adenoids. Eur J Radiol. 2011;79:38-41.
- [CrossRef] [PubMed] [Google Scholar]






