Translate this page into:
Pentazocine versus tramadol-paracetamol combination as analgesia in labor: A randomized controlled trial

*Corresponding author: Dennis Anthony Isah, Department of Obstetrics and Gynaecology, University of Abuja, University of Abuja Teaching Hospital, Abuja, Nigeria. denisanthonyisah@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Opadiran RO, Isah DA, Offiong R, Asudo FD. Pentazocine versus tramadolparacetamol combination as analgesia in labor: A randomized controlled trial. Ann Med Res Pract 2022;3:4.
Abstract
Objectives:
Labor should be a satisfactory experience and effective pain management should be employed as recommended by the American Congress of Obstetricians and Gynaecologists. In developing countries, pain management in labor is still a big challenge and the search for the ultimate labor analgesia is still ongoing. The objectives of the study were to determine whether the synergistic analgesic effect of the combination of tramadol and paracetamol will produce analgesia comparable to pentazocine with a better side effect profile.
Material and Methods:
This was a randomized controlled, double-blinded trial of tramadol-paracetamol combination versus pentazocine as labor analgesia and was carried out at the University of Abuja Teaching Hospital, Abuja, between June 2018 and March 2019. A total of 218 eligible parturients recruited at term, were counseled on labor analgesia, its benefits, and the options made available to them and educated on the pain scoring system. Parturients were allocated into two groups using computer-generated numbers with the WINPEPI software. Group A was given tramadol-paracetamol combination, while Group B received pentazocine, both at standard doses. Hourly pain scores, APGAR scores, labor duration, patients’ satisfaction, and side effects were collated. The level of significance was set at <0.05.
Results:
Tramadol-paracetamol was administered to 109 (50.9%) while pentazocine was administered to 105 (49.1%) of the study participants. The mean age in the tramadol-paracetamol group was 29.6 ± 4.8 years, and in the pentazocine group, it was 28.8 ± 4.5 years. The difference in pain scores on the visual analog scale was statistically significant at the 3rd and 4th h (P = 0.02 and 0.004), but not significant in the 1st and 2nd h (P = 0.05 and 0.22) in the two groups. Overall, the average pain score in the tramadol-paracetamol group was significantly higher compared to the pentazocine group (5.27 ± 1.86 vs. 4.72 ± 1.54; P = 0.02). The 1st and 5th min APGAR scores (P = 0.44 and 0.67, respectively) of neonates in the tramadol-paracetamol and pentazocine groups were comparable. Nausea and drowsiness occurred more frequently in the pentazocine group at P-values of 0.047 and 0.0015, respectively. There was no statistically significant difference in the duration of labor between the tramadol-paracetamol and pentazocine groups. not statistically significant, a higher proportion of parturients in the pentazocine group was satisfied compared with the tramadol-paracetamol group (71.4% vs. 63.3%; P = 0.13).
Conclusion:
This study showed that intravenous pentazocine provides better pain relief in labor, but the tramadol-paracetamol combination has fewer side effects.
Keywords
Tramadol
Pentazocine
Paracetamol
Labor
Analgesia
INTRODUCTION
Labor is one of the most painful physiological events a woman will experience in her lifetime.[1,2] Pain during labor varies in severity ranging from mild to severe pain.[1] However, in most individuals, it is described as severe particularly when labor has become advanced.[3] Worldwide, the adequacy of pain management is constantly being reviewed, as pain management in labor is not without its limitations. currently present, indeveloped countries, these limitations have been overcome to a large extent because because obstetricians are now aware of improved forms of labor analgesia. In order to achieve a satisfactory birth experience effective pain management should be employed as recommended by The American Congress of Obstetricians and Gynaecologists (ACOG).[4] Women in developed countries are also educated on the benefits of labor analgesia and are aware of the options available to them.[5] This allows them to choose the form of analgesia best suited to them.[5] Resources and skilled specialists are also readily available.[5]
However, in the developing countries such as Nigeria, there are multiple reasons why women are not availed of the opportunity of labor analgesia. This in part could be as a result of attitude of health-care personnel, limited resources, as well as sociocultural and religious beliefs of parturients and/or their relatives.[2,6] Available methods of labor analgesia include non-pharmacologic and pharmacologic methods.
Non-pharmacologic methods, such as hypnosis, acupuncture, and transcutaneous electrical nerve stimulation, among others, have been found useful in relieving labor pains. However, there are insufficient data on their efficacy in relieving pain during labor.[7]
Pharmacological methods such as epidural analgesia, inhalational agents, and systemic opioids have been found useful in relieving labor pains.[1,8-10]
Of these methods, epidural analgesia remains the gold standard as reported in various studies.[10,11] However, despite its effectiveness, it is underutilized in the developing countries including Nigeria mainly as a result of the cost, non-availability of drugs, equipment, and workforce in health facilities nationwide.[1]
Systemic opioids are commonly used as labor analgesia worldwide including Nigeria. They are readily available and accessible in Nigeria. They can be used as adjunct with subsequent initiation of epidural analgesia or as an independent method of analgesia. When used as a systemic analgesia, its use is limited to the first stage of labor due to their potential ability to cause respiratory depression in both the mother and the fetus and subsequently fetal distress. For this reason, repeated doses during the course of the first stage of labor is avoided.[12,11] Other side effects attributed to systemic opioids include behavioral and feeding problems which may last even up to 6 weeks following delivery apart from maternal side effects such as nausea, vomiting, sedation, and delayed gastric emptying.[10] Tramadol a systemic opioid, though not as effective as pentazocine has a unique advantage over other opioids in that is does not cause respiratory depression.[13] Paracetamol, a non-systemic opioid, has also been used as a labor analgesia but with varied efficacy.[8,14,15] Analgesics when used in combination have proven to have an improved efficacy.[16] Therefore, this study was aimed at determining whether the combination of tramadol and paracetamol can be of synergistic comparable efficacy with fewer side effects than pentazocine for labor analgesia.
MATERIAL AND METHODS
Study design
This was a randomized controlled trial of tramadolparacetamol combination versus pentazocine as labor analgesia.
Study population
The study population comprised all consenting women presenting to the labor ward in active phase of labor during the study period.
Inclusion criteria
Pregnant women at 37 weeks gestation–42 weeks admitted at cervical dilatation of 4–6 cm, who consented to the study.
Exclusion criteria
Parturient, who did not consent to the study, known allergy to pentazocine, paracetamol-tramadol, contraindication to vaginal delivery, pregnancy complicated by fetal distress, and intrauterine fetal death. Furthermore, maternal conditions such as cardiopulmonary depression, antepartum hemorrhage, history of recent/chronic liver disease, history of renal disease, diabetes mellitus, chronic hypertension, and those with prior analgesic administration were excluded from the study.
Sample size determination
Assuming a difference in mean pain score among groups of d= 0.87 17
S = standard deviation, 2.4 17
n = minimum sample size required for each group
Zα = standard normal deviate corresponding to a 95% confidence level, and level of 0.05 or 5%, which is 1.96
Zβ = power of the study to detect significant differences if it exists, at 95%, which is 1.64
The minimum sample size was 99 per group.
Considering 10% attrition rate,
Therefore, total sample size per group = 109 per group.
Thus, 109 parturients was allocated to each group giving a total of 218 parturients.
Informed consent
Parturient was counseled on the study and consent obtained. The counseling involved education on the need for research in the health sector to improve the standard of care. The benefits of obstetric analgesia were explicitly explained and parturients were assured of confidentiality. Parturients who refused participation were not denied care. There was no coercion.
Randomization and blinding
The study was double blinded such that both the parturients and the researcher were not aware of the medication, the participants were receiving. Eligible and consenting women were randomly assigned into two groups with the aid of the computer-generated numbers. The drugs were available at the obstetrics and gynecology pharmacy with number code corresponding to the appropriate regimen.
Groups
Tramadol-paracetamol combination group: Single dose of tramadol (TrabalinR) 1 mg/kg body weight, up to a maximum dose of 100 mg; and paracetamol (ParatexR) 15 mg/kg body weight and up to a maximum 1000 mg. Drugs were withdrawn from their vials into separate syringes and administered separately intravenously.
Pentazocine group: Single dose of pentazocine (FortwinR) 1 mg/kg body weight; up to a maximum dose of 60 mg/dose. This group also received a placebo (sterile water) as a second injection, which was the same volume as the paracetamol injection in the other group. As a result, both groups received two injections.
Instruments
Questionnaire: The researcher administered this and included details such as biodata, sociodemographic information, and previous side effects of drugs.
Questions and concerns raised were appropriately addressed. Data collection tool:
Following sensitization at the antenatal clinic, the women were enrolled at the labor ward. Informed consent was obtained and questionnaires were administered until sample size was attained. The assessment of the pain scoring system and Likert satisfaction scale was explained to the participants. Following administration of the assigned analgesia, the pain scoring was administered hourly till delivery. The satisfaction scale was also administered at delivery.
Subjects and methods
Awareness of this study was created among hospital staff at the antenatal clinic, maternity ward, and labor wards of the University of Abuja Teaching Hospital, Abuja.
All pregnant women at the antenatal clinic were counseled on the objectives of the study. On presentation at the labor ward, parturients were assessed and the study introduced to them. After they have understood and showed their willingness to be part of the study, an informed consent was obtained from them. Eligible parturients were then enrolled into the study. This procedure was followed until sample size was attained. The parturients were also educated on the pain scoring system (the visual analog pain score) and the Likert’s scale for maternal satisfaction.
Eligible parturients were randomly allocated into Group A or B. This randomization was done using computer-generated numbers by WINPEPI software by Abrahamson. Numbers generated were concealed in brown envelops, with the medication type enclosed within it. The researcher was solely responsible for the cost of purchasing the drugs and materials for the administration of the drugs. The midwife on duty with the help of the pharmacist in the obstetrics and gynecology pharmacy was responsible for withdrawing the medication from the vial ready for administration when requested. They were not involved in administering the pain score and satisfaction scale.
When parturients presented in labor, the departmental protocol was followed for their management. In addition, all eligible parturients were weighed and the weight in kilograms was used to calculate the appropriate drug dosage.
When confirmed that parturients were in the active phase of labor and cervical dilatation was between 4 and 6 cm, the participants either received the tramadol-paracetamol combination; tramadol 1 mg/kg body weight up to a maximum dose of 100 mg and 15 mg/kg body weight of paracetamol up to a maximum of 1000 mg; or pentazocine 1 mg/kg as a single dose up to a maximum dose of 60 mg, and sterile water in the second syringe.
However, in the course of the study, those that developed respiratory depression (if any) due to the effect of Pentazocine, which is defined as respiratory rate less than 12 cycles per minute in the adult, and tachypnea of greater than 60 cycles per minute with the evidence of in drawing chest wall and nasal flaring received intravenous naloxone, at a dosage of 0.4mg/ml. If there was no response in 2–3 min, the dose was to be repeated every minute until it reached a maximum of 10 mg, to reverse the effect. However, parturients who did require naloxone (if any) were dropped from the study as naloxone has the capacity to reverse the analgesic effect of pentazocine.
Following delivery, neonatal outcome was assessed using their APGAR scores, which were measured in the 1st and 5th min. Neonates noticed to be respiratory depressed following initial resuscitation were given naloxone at a dose of 0.1 mg/ kg.[7] Those who did not respond following administration of naloxone required admission into the special care baby unit (SCBU) and this was at the discretion of the neonatologist.
The administration of naloxone is, however, not recommended in the primary step of neonatal resuscitation and thus it was administered only when necessary. It was to be administered intravenously and in the absence of intravenous access, it was to be given intramuscularly.[7]
Parturients who developed nausea and vomiting following administration of tramadol or pentazocine were given parenteral promethazine at a dose of 25 mg stat. Through the course of labor, the visual analog scale was administered to the parturient hourly till delivery, side effects of the medications were also sought for, which included; nausea and vomiting, pruritus, and maternal respiratory distress, among others.
With the aid of a partograph, the duration of labor was measured from the time of admission into the labor ward in active phase of labor as well as the cervical dilatation at presentation. The time of delivery was also noted.
Following delivery, the Likert satisfaction scale was administered to assess the analgesic satisfaction of the parturients.
Statistical analysis
Data analysis was done using the Statistical Package for the Social Sciences version 20. Descriptive analyses were conducted to examine the sociodemographic characteristics of women in both groups, and the results were presented in tables and charts. Groups were compared using t-test and Chi-square test. P < 0.05 was considered statistically significant at a 95% confidence interval.
Ethical clearance
The study commenced after obtaining approval from the University of Abuja Teaching Hospital Research Ethics Committee.
RESULTS
Two hundred and fifty women were assessed for eligibility, out of which 218 were recruited based on the prior sample size calculation. Complete case analysis was done, excluding participants with missing data, and yielding a final sample size of 214.
[Table 1] shows the sociodemographic characteristics of the respondents. The average age of women in the sample was 25 ± 4.6 years, with the age ranging from 18 to 43 years. About 38% of parturients in the study sample were between the ages of 25 and 29. Between the tramadol-paracetamol and pentazocine group, there were no statistically significant differences in all the sociodemographic characteristics, except parity which had P = 0.03.
| Variables | Tramadol-paracetamol n(%) | Pentazocine n(%) | Test | P-value | Total n(%) |
|---|---|---|---|---|---|
| Age | |||||
| <25 | 23 (21.0) | 21 (20.0) | χ2=4.14 | 0.25 | 3 (1.4) |
| 25–29 | 28 (25.7) | 40 (38.1) | 27 (12.6) | ||
| 30–34 | 42 (38.5) | 45 (42.9) | 82 (38.3) | ||
| ≥35 | 16 (14.7) | 33 (31.4) | 75 (35.1) | ||
| Mean age | 29.6 ± 4.8 | 28.8 ± 4.5 | t=1.30 | 0.19 | 27 (12.6) |
| Tribe | |||||
| Yoruba | 12 (11.0) | 14 (13.3) | χ2=2.45 | 0.48 | 26 (12.2) |
| Hausa | 16 (14.7) | 22 (21.0) | 38 (17.8) | ||
| Igbo | 24 (22.0) | 17 (16.2) | 41 (19.2) | ||
| Others | 57 (52.3) | 52 (49.5) | 108 (50.9) | ||
| Educational level | |||||
| Informal | 10 (9.2) | 13 (12.4) | χ2=1.51 | 0.68 | 23 (10.8) |
| Primary | 9 (8.3) | 5 (4.8) | 14 (6.5) | ||
| Secondary | 34 (31.2) | 33 (31.4) | 67 (31.3) | ||
| Tertiary | 56 (51.4) | 54 (51.4) | 110 (51.4) | ||
| Occupation | |||||
| Unemployed | 29 (26.6) | 31 (29.5) | χ2=1.18 | 0.88 | 60 (28.0) |
| Trader/artisan | 26 (23.9) | 20 (19.1) | 46 (21.5) | ||
| Civil servant | 20 (18.4)) | 23 (21.9) | 43 (20.1) | ||
| Student | 10 (9.2) | 10 (9.5) | 20 (9.4) | ||
| Others | 24 (22.0) | 21 (20.0) | 45 (21.0) | ||
| Parity | |||||
| 0 | 31 (28.4) | 47 (44.8) | χ2=7.21 | 0.03 | 78 (36.5) |
| 1–4 | 72 (66.1) | 56 (53.3) | 128 (59.8) | ||
| >4 | 6 (5.5) | 2 (1.9) | 8 (3.7) | ||
| Booking status | |||||
| Unbooked | 3 (2.8) | 2 (1.9) | χ2=0.46 | 0.79 | 5 (2.3) |
| Booked | 99 (90.8) | 98 (93.3) | 197 (92.1) | ||
| Booked elsewhere | 7 (6.4) | 5 (4.8) | 12 (5.6) | ||
| Total | 109 (50.9) | 105 (49.1) | 214 (100) |
[Table 2] shows the mean pain scores in the tramadolparacetamol and pentazocine groups at various time intervals. The mean pain scores were higher at all time intervals in the tramadol-paracetamol group compared with the pentazocine group. The observed difference in mean pain scores was statistically significant between the tramadol-paracetamol and pentazocine groups at the 3 h and 4 h intervals.
| Pain scores | Tramadol-paracetamol Mean±SD | Pentazocine Mean±SD | t-test statistic | P-value |
|---|---|---|---|---|
| At 1 h | 4.30±3.29 | 3.72±1.84 | 1.98 | 0.05 |
| At 2 h | 4.81±2.09 | 4.49±1.72 | 1.22 | 0.22 |
| At 3 h | 5.62±1.94 | 5.03±1.83 | 2.28 | 0.02 |
| At 4 h | 6.35±1.84 | 5.64±1.78 | 2.89 | 0.004 |
| Overall | 5.27±1.86 | 4.72±1.54 | 2.35 | 0.02 |
As shown in [Table 3], 1 (0.9%) neonate in the tramadolparacetamol group and 3 (2.9%) neonates in the pentazocine groups were admitted to the SCBU. The indications were instrumental vaginal delivery, perinatal asphyxia, and small for gestational age. There was no statistically significant difference in admission to SCBU, between the tramadolparacetamol and pentazocine groups. A Mann–Whitney U-test was run to determine if there were differences in the 1st and 5th min median APGAR scores between the tramadol-paracetamol and pentazocine groups; there was no statistically significant difference.
| Tramadol/paracetamol | Pentazocine | Test statistic | P-values | |
|---|---|---|---|---|
| Admission to SCBU | ||||
| Yes | 1 (0.9) | 3 (2.9) | 0.36* | |
| No | 108 (99.1) | 102 (97.1) | ||
| APGAR score at 1 min | ||||
| <7 | 7 (6.4) | 10 (9.5) | χ2=0.71 | 0.40 |
| ≥7 | 102 (93.6) | 95 (90.5) | ||
| APGAR score at 5 min | ||||
| <7 | 1 (0.9) | 3 (2.9) | 0.36* | |
| ≥7 | 108 (99.1) | 102 (97.1) | ||
| Median APGAR score | ||||
| 1st min | 8.0 | 8.0 | U=5395 U=5542 | 0.44 |
| 5th min | 9.0 | 9.0 | 0.67 |
[Table 4] shows the condition of respondents in the two groups, with regard to side effects and the mode of delivery. In the tramadol-paracetamol group, 66 (60.6%) respondents did not report any side effects, compared with 50 (47.6%) respondents in the pentazocine group. Overall, 39.5% of parturients in the tramadol-paracetamol group reported one side effect compared to 52.4% in the pentazocine group. The most frequently reported side effect was dizziness (14.7%) in the tramadol-paracetamol group and drowsiness (19.1%) in the pentazocine group. The difference in occurrence of side effects between the two groups was statistically significant for nausea (P = 0.047) and drowsiness (P = 0.015). Parturients in the pentazocine group had 2.6 times the risk of nausea compared to those in the pentazocine group. Furthermore, the risk of drowsiness was 3 times more in the pentazocine group compared to the tramadol-paracetamol group.
| Tramadol-paracetamol | Pentazocine | RR | P-value | |
|---|---|---|---|---|
| Side effects | ||||
| Nausea | 6 (5.5) | 13 (12.4) | 2.6 | 0.047 |
| Vomiting | 5 (4.6) | 2 (1.9) | 0.58 | 0.456 |
| Drowsiness | 9 (8.3) | 20 (19.1) | 3 | 0.015 |
| Dizziness | 16 (14.7) | 16 (15.2) | 1.23 | 0.488 |
| Others | 7 (6.4) | 4 (3.8) | 0.80 | 0.666 |
| None | 66 (60.6) | 50 (47.6) | 1 | |
| Mode of delivery | ||||
| Vaginal delivery | 106 (97) | 102 (97.1) | 1 | |
| Emergency cesarean section | 1 (0.92) | 2 (1.9) | 1.89 | 0.553 |
| Assisted vaginal delivery | 2 (1.8) | 1 (1.0) | 0.53 | 0.595 |
Pentazocine is compared to tramadol-paracetamol combination; the relative risk (RR) values in the table above are for pentazocine
The most frequent mode of delivery in the two groups was spontaneous vaginal delivery; 97% in the tramadol-paracetamol combination group and 97.1% in the pentazocine group. Emergency cesarean section accounted for <1% in the tramadol-paracetamol group and 1.9% in the pentazocine group. The difference in modes of delivery between the two groups was not statistically significant.
[Table 5] shows the duration of the stages of labor in the tramadol-paracetamol and pentazocine groups. The median duration of labor in the first stage (active) was 4.36 h in the two groups. However, the difference was not statistically significant (P = 0.61). In all the stages of labor, the observed difference in the duration of labor between the groups was not statistically significant.
| Stages of labour | Tramado-Paracetamol Median | Pentazocine Median | Mann-Whitney U | P-Value |
|---|---|---|---|---|
| Active First stage(stage) 4.36 | 4.36 | 4.36 | 5490 | 0.61 |
| Second stage (minutes) 20.0 | 20.0 | 20.0 | 5700 | 0.96 |
| Third stage (minutes) 5.0 | 5.0 | 7.0 | 5348 | 0.40 |
| Overall duration 5.31 | 5.31W | 5.27 | 5371 | 0.44 |
Maternal satisfaction scores for both groups are illustrated in [Figure 1]. Women in the pentazocine group (71.4%) were generally more satisfied compared to those in the tramadolparacetamol group (63.3%). About 6.5% of respondents in the tramadol-paracetamol group were dissatisfied compared with 2% in the pentazocine group. A Mann–Whitney U-test was run to determine if there were differences in satisfaction scores between the tramadol-paracetamol and pentazocine groups. There were no statistically significant differences between the groups, P = 0.13, as shown in [Figure 2].

- Maternal satisfaction scores in the tramadol-paracetamol and pentazocine groups.
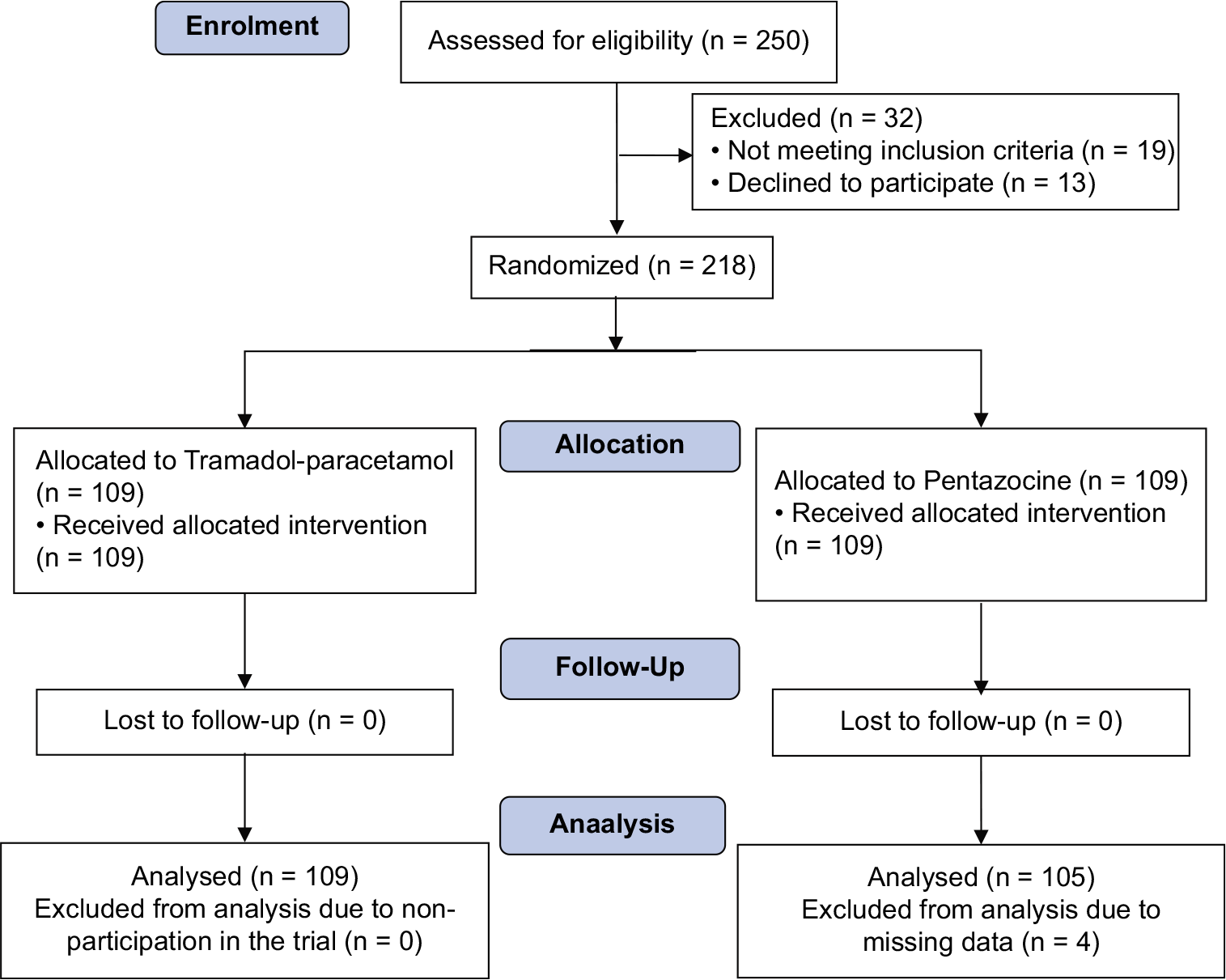
- Flow of participants through the phases of the randomized trial of the tramadol-paracetamol and pentazocine groups. Adapted from Consort, 2010.
DISCUSSION
The current study examined and compared the efficacy of tramadol-paracetamol combination and pentazocine for labor analgesia. Based on researcher’s knowledge, there is a paucity of studies in which pentazocine was compared to tramadol-paracetamol combination for labor analgesia. However, other studies have compared the analgesic efficacy of pentazocine to other opiates, paracetamol, or placebo for analgesia in labor.
Results of the present study revealed that the baseline sociodemographic characteristics of parturients in the two groups were similar. Parturients that were booked were more than those that were unbooked. This may be because the study is hospital based. This was comparable with findings from Makkar et al. (2015)[15] and Aimakhu et al. (2017),[18] where the analgesic efficacy of paracetamol and tramadol in labor was compared, showed in their studies that booked patients were more than unbooked patients, while other baseline sociodemographic characteristics were similar in both groups. Tertiary education was the most frequent level of education observed in the study sample; this may be because the study area includes tertiary institutions and government parastatals. Furthermore, there were more multiparous women than primipara or grand multipara. Results from other studies have also showed a higher proportion of multiparous women and tertiary educated women in their study sample.[17,18]
Women in both groups experienced moderate pain relief all through the 4 h that pain was assessed. This shows that pentazocine and tramadol-paracetamol combination are equally effective for pain relief during labor, as the combination of tramadol-paracetamol leads to a synergistic mechanism that increased its efficacy,[16,19] making its effect comparable to pentazocine. Labor pain can be considered a severe pain, which can be managed with strong analgesics such as pentazocine or other opioids.[16,19] Due to the IV administration, the first pass effect in the liver is by-passed leading to higher tissue concentration of the drugs, which enhances the analgesic effect of the drug.[20] Some studies have shown that pentazocine and tramadol are equally effective as pain relief in labor.[13]
Average pain scores and overall mean pain score were significantly lower among women who received pentazocine compared to women who received tramadol-paracetamol. Pentazocine was noticed to have a considerable sedative effect, making them report lower pain scores at all hours of pain assessment. Furthermore, in the hours following administration of the drugs, the average pain scores increased in both groups, this may be due to single-dose administration of the different medications and the drug clearance with time. It has been reported that the onset of action of pentazocine is about 15 min, and it acts for 4–5 h; tramadol peaks after 2 h of administration, and the time to peak effect for paracetamol is 1.5–3 h.[21-23] Pentazocine acts quicker than paracetamol and tramadol but the peak action times of all the medications seem similar, which may explain why the mean pain scores at 2 h in both groups were not different.
This finding is comparable with the results from Ekweani et al. (2014) who compared pentazocine with acetaminophen and found that pentazocine had better analgesic efficacy.[17] Some other studies have also found that pentazocine has better analgesic efficacy than tramadol.[20,24,25] Shetty et al. (2014), in their study that compared tramadol with pentazocine, found that pain relief toward the end of first stage of labor was inadequate in both groups, though more women in the pentazocine group reported moderately severe pain compared to the tramadol group who reported severe pain.[13]
The APGAR scores and the need for SCBU admission were statistically comparable in the tramadol-paracetamol and pentazocine groups. Opiates can cross the placental barrier and cause respiratory depression in neonates,[17] but this may have been unlikely in this study as single dose of medications may have limited the possibility of neonatal respiratory depression. The indications observed for SCBU admission in this study were perinatal asphyxia due to instrumental vaginal delivery in delayed second stage and small for gestational age. This was a similar finding in some other studies, where no significant difference was found between pentazocine and tramadol or pentazocine and acetaminophen, for neonatal outcomes.[13,17,20,24,27]
Regarding maternal side effects, pentazocine caused more side effects in the parturients, than tramadolparacetamol, being that it is a stronger opioid and has more sedative effect than tramadol. It inhibits the ascending pathways, leading to alteration in response to pain, producing analgesia and sedation.[28] Other studies have found higher incidence of drowsiness and sedation in pentazocine compared with the likes of paracetamol or tramadol.[17,20,26,27] However, the sedative effect of pentazocine may be helpful in calming anxious parturient, particularly primigravidae.[17,25] Furthermore, duration of labor may be prolonged in parturients who received pentazocine compared to those who received tramadol-paracetamol as was observed in the present study. The sedative effect of pentazocine may have led to decreased mobility and uprightness, thus increasing duration of labor. Studies on mother’s position and mobility during the first stage of labor have shown that labor may be shorter for women who are upright and walk around.[29] Similarly, Chandnani and Sainee (2013), in their study comparing pentazocine and tramadol for pain relief in labor, found that labor duration did not increase after the use of tramadol, but it increased with pentazocine.[26] Tripti and Jyotsna (2006) also found shorter duration of labor with tramadol compared to pentazocine.[24]
The level of satisfaction was similar among parturients that received pentazocine and those who received tramadolparacetamol. This may be attributed to the similarity in level of pain relief that parturients in both groups experienced, since the combination of tramadol-paracetamol leads to a synergistic mechanism that can increase its efficacy,[16,19] comparable to that of pentazocine. However, a Cochrane systematic review compared maternal satisfaction with labor pain relief as a secondary outcome, between opioid and nonopioid analgesics, women who received opioid analgesics were more likely to be satisfied than their counterparts who had non-opioid analgesics.[11] This may be due to the sedative effect of opioids.[25]
CONCLUSION
This study showed that intravenous pentazocine provided better pain relief than intravenous tramadol-paracetamol combination. Furthermore, neonatal adverse effects, labor duration, and maternal side effects were comparable in the tramadol-paracetamol combination and pentazocine groups. Maternal satisfaction with pain relief during labor was higher among parturients who received pentazocine compared with tramadol-paracetamol combination, though not statistically significant.
In view of this, it can be concluded that pentazocine provides better pain relief in labor, but tramadol-paracetamol combination has a better safety profile.
Acknowledgment
I wish to appreciate the Chief Medical Director Professor BA Ekele, Professor AY Isah, and Head of Department Associate Professor ET Agida for their fatherly roles and mentorship.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Pain relief in labor: A survey of awareness, attitude, and practice of health care providers in Zaria, Nigeria. J Pain Res. 2011;4:227-32.
- [CrossRef] [PubMed] [Google Scholar]
- Obstetric analgesia for vaginal birth in contemporary obstetrics: A survey of the practice of obstetricians in Nigeria. BMC Pregnancy Childbirth. 2014;14:140.
- [CrossRef] [PubMed] [Google Scholar]
- Intravenous paracetamol versus intramuscular pethidine in relief of labour pain in primigravid women. Niger Med J. 2014;55:54-7.
- [CrossRef] [PubMed] [Google Scholar]
- ACOG Committee on Practice Bulletins-Obstetrics. ACOG practice bulletin. Clinical management guidelines for obstetrician-gynecologists number 36 July 2002. Obstetric analgesia and anesthesia. Obstet Gynecol. 2002;100:177-91.
- [CrossRef] [PubMed] [Google Scholar]
- More in hope than expectation: A systematic review of women's expectations and experience of pain relief in labour. BMC Med. 2008;6:7.
- [CrossRef] [PubMed] [Google Scholar]
- Basis of obstetric analgesia and anaesthesia during childbirth. Internet J Health. 2008;9:1-9.
- [CrossRef] [Google Scholar]
- Labour analgesia: Recent advances. Indian J Anaesth. 2010;54:400-8.
- [CrossRef] [PubMed] [Google Scholar]
- Intravenous infusion of paracetamol versus intravenous pethidine as an intrapartum analgesic in the first stage of labor. Int J Gynecol Obstet. 2012;118:7-10.
- [CrossRef] [PubMed] [Google Scholar]
- Butorphanol in labour analgesia: A prospective cohort study. J Turk Ger Gynecol Assoc. 2013;14:221-4.
- [CrossRef] [PubMed] [Google Scholar]
- Analgesia in labour: Induction and maintenance. Anaesth Intensive Care Med. 2013;14:276-9.
- [CrossRef] [Google Scholar]
- Non-opioid drugs for pain management in labour. Cochrane Database Syst Rev. 2012;7:CD009223.
- [CrossRef] [Google Scholar]
- Labour analgesia when epidural is not a choice: Tramadol versus pentazocine. ISRN Obstet Gynecol. 2014;2014:930349.
- [CrossRef] [PubMed] [Google Scholar]
- Intravenous paracetamol infusion versus intramuscular tramadol as an intrapartum labor analgesic. J Obstet Gynaecol India. 2015;65:17-22.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of analgesic efficacy of paracetamol and tramadol for pain relief in active labor. J Clin Anesth. 2015;27:159-63.
- [CrossRef] [PubMed] [Google Scholar]
- Tramadol/paracetamol fixed-dose combination: A review of its use in the management of moderate to severe pain. Clin Drug Investig. 2010;30:711-38.
- [CrossRef] [PubMed] [Google Scholar]
- A comparative study of intramuscular acetaminophen versus intramuscular pentazocine as labour analgesia in zaria, Northwestern nigeria. J West Afr Coll Surg. 2014;4:35-53.
- [Google Scholar]
- Pain relief in labour: A randomized controlled trail comparing intramuscular tramadol with intramuscular para ceutamol at the university college hospital Ibadan Nigeria. Trop J Obstet Gynaecol. 2017;34:91-8.
- [CrossRef] [Google Scholar]
- Dose response of tramadol and its combination with paracetamol in UVB induced hyperalgesia. Eur J Pain. 2012;16:562-73.
- [CrossRef] [PubMed] [Google Scholar]
- Arandomized controlled trail of intramuscular pentazocine compared to intravenous paracetamol for pain relief in labour at Amino Kano Teaching Hospital, Kano. Trop J Obstet Gynaecol. 2017;34:116-23.
- [CrossRef] [Google Scholar]
- The pharmacokinetics of pentazocine and tripelennamine. Clin Pharmacol Ther. 1986;39:669-76.
- [CrossRef] [PubMed] [Google Scholar]
- Tramadol: A new centrally acting analgesic. Am J Health Pharm. 1997;54:643-52.
- [CrossRef] [PubMed] [Google Scholar]
- Metabolism and disposition of acetaminophen: Recent advances in relation to hepatotoxicity and diagnosis. Pharm Res. 2013;30:2174-87.
- [CrossRef] [PubMed] [Google Scholar]
- Pain relief in labour-tramadol versus pentazocine. J Obstet Gynaecol India. 2006;56:406-9.
- [Google Scholar]
- Pain relief in labour: A randomized controlled trail comparing pentazocine with Tramadol. Niger J Obstet Gynaecol. 2008;3:14-8.
- [CrossRef] [Google Scholar]
- Pain relief in labour: Tramadol versus pentazocine. Int J Reprod Contracept Obstet Gynecol. 2013;2:186.
- [CrossRef] [Google Scholar]
- Pentazocine Hydrochloride Prescribing Information Version 2.0. 2017. Available from: http://www.druglib.com/druginfo/tawin/description_pharmacology [Last accessed on 2017 Oct 20]
- [Google Scholar]
- Maternal positions and mobility during first stage labour. Cochrane Database Syst Rev. 2013;10:CD003934.
- [CrossRef] [Google Scholar]






