Translate this page into:
Intralesional cryotherapy – A pilot study of African treated for keloids plastic surgery

*Corresponding author: Samuel Okpechi, Department of Surgery, University of Abuja Teaching Hospital, Gwagwalada, Abuja. drokpechisamuel@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Abubakar A, Okpechi S. Intralesional cryotherapy – A pilot study of African treated for keloids plastic surgery. Ann Med Res Pract 2020;1:2.
Abstract
Objective:
There is a high prevalence of keloids among Africans and Asians. It is a huge burden on the public health system. This presentation is a pilot study on the effectiveness of intralesional cryotherapy in treating keloids in African.
Material and Methods:
Eleven patients were recruited from the surgical outpatient department and treated with a single exposure of intralesional cryotherapy. They were monitored for 12 months.
Results:
The 11 patients were treated with 12 keloid lesions. The patients consisted of seven males (63.6%) and four females (36.4%). Their age ranged from 18 years to 45 years. The chest region accounted for 46.6%, the head and neck was 46.7%, and the mons pubis 6.7%. In 1 year of follow-up, ten patients had total resolution of symptoms, while one patient did not have any improvement of symptoms.
Conclusion:
The treatment of keloid thus far has continued to be a challenge to both the African and the doctors. Intralesional cryotherapy presents a novel way of treatment that holds a lot of promise for the African.
Keywords
Cryotherapy
African
Keloids
INTRODUCTION
Keloids are cosmetically disfiguring benign fibrous outgrowths, which present as a major therapeutic dilemma due to their frequent recurrence.[1,2]
Keloids have affected patients and a source of frustration for treating surgeons. They result from excessive collagen deposits, etiology of which remains elusive and commonly affect 4.5–16% of the general population.[3,4]
The etiology of keloids remains unknown. Although it is suggested that a relation exists with wound tension, sex hormones, sebaceous gland activity, melanocyte concentration in the overlying keratinocytes, and genetic predisposition, no single theory has proven in all aspects of keloids.[5-7]
The highest incidence is seen in patients with darker skin, whereas the Mediterranean, South Americans, and Asians are slightly less affected, and Caucasians are the least affected (<1%).[6,8]
Patients at high risk of keloids are usually younger than 30 years. The sternal skin, shoulders and upper arms, earlobes, and cheeks are most susceptible to developing keloids following wound healing.[2] High-risk trauma includes burns, ear piercing, and any factor that prolongs wound healing.[1,3]
Keloids are often visible on earlobes or so large that they are visible through clothing, which becomes a major psychosocial burden. Keloids also give rise to pain and pruritus in 80% of keloid patients.[6,8,9]
Keloids have been shown to respond to excision, radiation, pressure therapy, intralesional corticosteroids, interferon and fluorouracil therapy, topical silicon and dressings, and pulse dye laser treatment.[10] All of these have been shown to be associated with some percentages of recurrence.[3,4,10-15]
Cryotherapy (CryoShape[16]) is a safe and effective treatment of keloids. Intralesional cryosurgery has been shown to bring about significant improvement in keloids.[17]
Melanocytes, the cells that produce skin pigments, are located more at the surface of the skin and are sensitive to extremely cold temperatures. The intralesional method has been shown to result in more moderate but longer-lasting temperature reductions. Contrasting with contact and spray therapies, with this method, the tissue area that gets the coldest is inside the scar, further away from the scar surface and is less likely to kill off melanocytes.[18]
The first true cryosurgery was performed in the late 19th century by a dermatologist Campbell White who used solid CO2 as a cryogen.[19-21] Liquid nitrogen with a boiling point of −196°C is the most widely used. Cryogens can be delivered to the tissues in various ways, for example, cryoprobes and open spray nozzles of variable sizes with which a very fine control can be achieved. The spray is emitted from a distance of 1–2 cm from the target site and at a 90 degree angle to it. This therapeutic modality makes use of local freezing for controlled destruction or removal of living tissues.[18,22,23]
This study aims to report the outcome of intralesional cryotherapy on African. The objectives are to find a more effective means of treating keloids in the black race and to in the long-term reduce the burden of treating recurrence on the public health system.
MATERIAL AND METHODS
This is a report on the progress of 11 patients who were consecutively selected at the plastic surgery outpatient clinic. No exclusion criteria were excluded from the study.
Ethical clearance obtained and consent forms duly were signed by the patients before the procedure.
Materials for intralesional cryotherapy included cryoprobe (Etgar Group International Limited) [Figure 1] which was attached to a 500 ml canister of liquid nitrogen, anesthetic agent, plasters, antibiotic ointment, and sterile gauze.
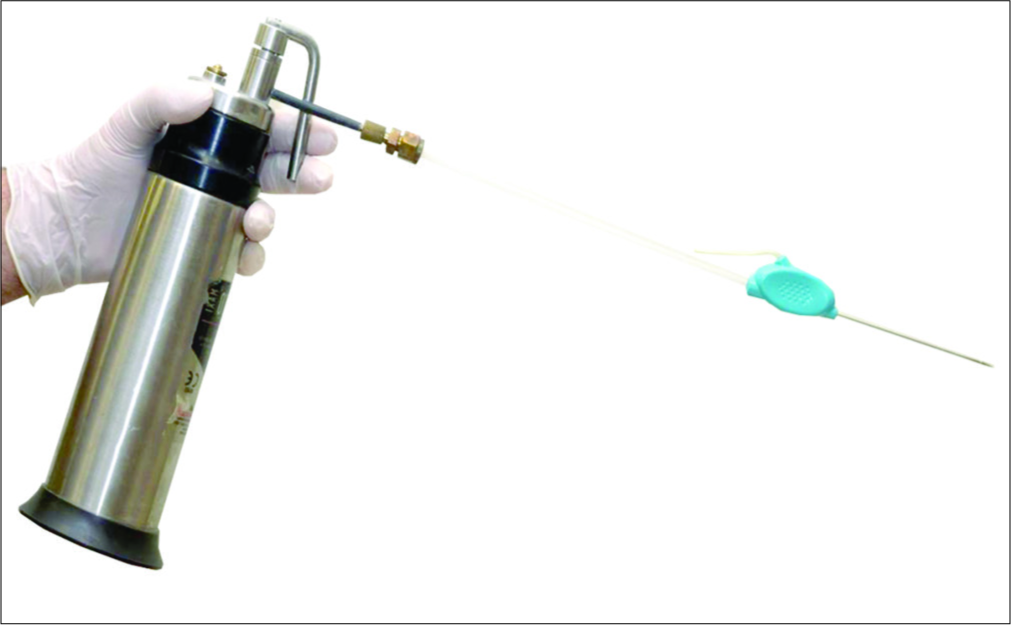
- Cryotherapy probe and liquid nitrogen canister.
Technique
After cleaning the keloid with disinfectant [Figure 2], the scar and underlying tissue infiltrated with the local anesthetic.

- Auricular keloid before cryotherapy.
The keloid is pinched with one hand, while the cryoprobe is pushed into the scar about 5 mm below the surface and run parallel across the longest axis of the scar until it reaches the other sides.
The liquid nitrogen gas is released, and ice balls [Figure 3] will form along with the probe until the keloid is completely frozen.

- Auricular keloid with ice ball immediately after cryotherapy.
The flow of liquid nitrogen is stopped, and the probe is left in the keloid for a couple of minutes to thaw before it is taken out.
Sterile gauze is applied to the keloid to cover the penetration sites.
The keloid is cleaned twice a day with warm water and an antibiotic ointment applied until fully healed.[18]
RESULTS
Intralesional cryotherapy was done for11 patients; each patient had one exposure. The sex distribution was seven (63.65) males and four (36.4%) females aged from 18 years to 45 years. The keloids were distributed thus: Three on the scalp (13.3%), three on the face (20%), one on the ear (6.7%), seven on the chest with five on the sternum, one on the infraclavicular region (46.7%), one on the breast (6.7%), and one on the mons pubis (6.7%) [Table 1]. Five patients had two or more keloids treated. Each patient had several follow-up visits with good flattening of the scars, absent pain, and itching on scars and improvement of pigmentation [Figure 4]. All patients had hypopigmentation along the needle tract which subsided with follow-up. One patient reported no improvement in his symptoms. There is no report of recurrence in the patients that responded 12 months after the procedure [Table 1].

- Eighteen months after cryotherapy.
| Location | Number of keloids | Percentage |
|---|---|---|
| Scalp | 2 | 13.3 |
| Ear | 1 | 6.7 |
| Face | 3 | 20 |
| Chest | 7 | 46.6 |
| Breast | 1 | 6.7 |
| Mons pubis | 1 | 6.7 |
| Total | 15 | 100 |
DISCUSSION
This was an observational study and a pilot to a larger study. It is the first study that consisted of all dark-skinned patients and the first in Nigeria. The burden of keloids in the black African race has been put at 6–16%[24] with the general rate of recurrence of 60–80% after surgical treatment.[25]
The treatment for keloids has been legion from intralesional corticosteroids which were regarded as the best, which inhibits alpha-2 macroglobulin with the treatment running over 6 months.[26] Other injectables include 5FU, triamcinolone, and bleomycin either individually or as combined therapy. All of these involve several injections over the treatment course. Although surgical excision of keloids leads to an immediate esthetic outcome,[27] as a monotherapy, it has a 70% recurrence rate.[26] Surgery also has added risks from anesthesia and the surgical risks.[27] Shepard and Daeber, in 1982, were the first to record success in the use of cryotherapy in the treatment of keloids. They used contact cryotherapy, though treatment was successful patients that were left with residual skin hypopigmentation.[28] It was also followed by a 30% recurrence rate; thus, this method was relegated to the archives until Mende[29] and Zouboulis and Orfanos[30] in their studies showed that repeat contact cryotherapy resulted in decreased cases of recurrence. Intralesional cryotherapy was first developed to avoid the complications of the conventional method.[31] This method was further refined by Prof. Har-Shai,[32] this study was modeled after it.
The success rate recorded with intralesional cryotherapy has been documented mainly in the Caucasians with a zero percent recurrence in 18 months.[26] The complications recorded in patients treated with contact cryotherapy, which include skin atrophy and hypopigmentation[33] were reduced with the use of the CryoShape probe. These complications are worse in darker skin.[34]
In this study, all of our patients were African. The temporary skin changes reported by Gupta et al. were recorded, but this resolved in 12 months. The patients recorded relief of all symptoms – itching, pain, and enlargement. The largest keloid [Figure 2] had flattened in 4 months, and pigmentation had normalized in 12 months [Figure 4].
Studies have should keloids to have a recurrence rate of up to 75% within 12 months of treatment,[35,36] none of the patients in this study had recurrence during follow-up. It has been observed that intralesional cryotherapy cases pathological scar tissue induce the differentiation of abnormal keloidal fibroblasts toward a normal phenotype.[37] This leads to the fibroblast shifting toward a higher ratio of collagen III to collagen I.
CONCLUSION
The burden of keloids in Africa has been stated by several authors.[38-40] Intralesional cryotherapy may offer a solution to the multitude of keloid patients of African descent, as reflected in this pilot study. A larger study is necessary to explore the full benefit of this treatment option.
Acknowledgment
The Federal Ministry of health for organizing training on intralesional cryotherapy, Prof Yaron Har-Shai for an enlightening demonstration, Dr. Richard Nnabuko, and Dr. Ramatu Hassan for facilitating the training.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Keloid histopathology after intralesional cryosurgery treatment. J Eur Acad Dermatol Venereol. 2011;25:1027-36.
- [CrossRef] [PubMed] [Google Scholar]
- Keloid or hypertrophic scar: The controversy: Review of the literature. Ann Plast Surg. 2005;54:676-80.
- [CrossRef] [PubMed] [Google Scholar]
- Keloids: Clinical features and management. Part II. J Pak Assoc Derma. 2006;16:163-72.
- [Google Scholar]
- Keloidal scars: A review with a critical look at therapeutic options. J Am Acad Dermatol. 2002;46:S63-97.
- [CrossRef] [PubMed] [Google Scholar]
- Intralesional cryotherapy versus excision and corticosteroids or brachytherapy for keloid treatment: Study protocol for a randomised controlled trial. Trials. 2013;14:439.
- [CrossRef] [PubMed] [Google Scholar]
- Hypertrophic scars and keloids--a review of their pathophysiology, risk factors, and therapeutic management. Dermatol Surg. 2009;35:171-81.
- [CrossRef] [PubMed] [Google Scholar]
- Keloids: Current concepts of pathogenesis (review) Int J Mol Med. 2009;24:283-93.
- [CrossRef] [PubMed] [Google Scholar]
- On the nature of hypertrophic scars and keloids: A review. Plast Reconstr Surg. 1999;104:1435-58.
- [CrossRef] [PubMed] [Google Scholar]
- The hidden cost of skin scars: Quality of life after skin scarring. J Plast Reconstr Aesthet Surg. 2008;61:1049-58.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of the keloid: What is new? Otolaryngol Clin North Am. 2002;35:207-20, 8
- [CrossRef] [Google Scholar]
- Pain evaluation and control during and following the treatment of hypertrophic scars and keloids by contact and intralesional cryosurgery--a preliminary study. J Eur Acad Dermatol Venereol. 2012;26:440-7.
- [CrossRef] [PubMed] [Google Scholar]
- Intralesional vs. contact cryosurgery in treatment of keloids: A clinical and immunohistochemical study. Int J Dermatol. 2015;54:468-75.
- [CrossRef] [PubMed] [Google Scholar]
- Keloids in various races. A review of 175 cases. Plast Reconstr Surg. 1969;44:564-6.
- [CrossRef] [PubMed] [Google Scholar]
- Essential Tissue Healing of the Face and Neck. (1st ed). USA: Shelton People's Medical publishing House; 2009. p. :95-212.
- [Google Scholar]
- Description of site-specific morphology of keloid phenotypes in an Afrocaribbean population. Br J Plast Surg. 2004;57:122-33.
- [CrossRef] [PubMed] [Google Scholar]
- Intralesional cryotherapy for enhancing the involution of hypertrophic scars and keloids. Plast Reconstr Surg. 2003;111:1841-52.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of cryosurgery in keloids and hypertrophic scars. A prospective consecutive trial of case series. Arch Dermatol. 1993;129:1146-51.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of skin surface temperature on skin pigmentation during contact and intralesional cryosurgery of keloids. J Eur Acad Dermatol Venereol. 2007;21:191-8.
- [CrossRef] [PubMed] [Google Scholar]
- Hypertrophic scars and keloids: Etiology and management. Am J Clin Dermatol. 2003;4:235-43.
- [CrossRef] [PubMed] [Google Scholar]
- Intralesional cryosurgery enhances the involution of recalcitrant auricular keloids: A new clinical approach supported by experimental studies. Wound Repair Regen. 2006;14:18-27.
- [CrossRef] [PubMed] [Google Scholar]
- Update on the Management of Keloids. Seminars in Cutaneous Medicine and Surgery. 2009;28:71-6.
- [CrossRef] [PubMed] [Google Scholar]
- Intralesional cryotherapy versus excision with corticosteroid injections or brachytherapy for keloid treatment: Randomised controlled trials. J Plast Reconstr Aesthet Surg. 2018;71:847-56.
- [CrossRef] [PubMed] [Google Scholar]
- The response of keloid scars to cryosurgery. Plast Reconstr Surg. 1982;70:677-82.
- [CrossRef] [PubMed] [Google Scholar]
- Kryochirurgische behandlung von hyper trophen narben und keloiden. Hautarzt. 1990;41:683-8.
- [Google Scholar]
- Intralesional cryosurgery. A new technique using cryoneedles. J Dermatol Surg Oncol. 1993;19:123-6.
- [CrossRef] [PubMed] [Google Scholar]
- The intralesional cryosurgery technique a new and effective technology for the treatment of hypertrophic scars and keloids d. Scar J. 1982;510:1-11.
- [Google Scholar]
- Current developments and uses of cryosurgery in the treatment of keloids and hypertrophic scars. Wound Repair Regen. 2002;10:98-102.
- [CrossRef] [PubMed] [Google Scholar]
- Intralesional cryosurgery using lumbar puncture and/or hypodermic needles for large, bulky, recalcitrant keloids. Int J Dermatol. 2001;40:349-53.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of keloids by combined surgical excision and immediate postoperative X-ray therapy. Ann Plast Surg. 1981;7:281-5.
- [CrossRef] [PubMed] [Google Scholar]
- Cryotherapy modifies synthetic activity and differentiation of keloidal fibroblasts in vitro. Exp Dermatol. 2003;12:673-81.
- [CrossRef] [PubMed] [Google Scholar]
- Demographic and clinical characteristics of keloids in an urban center in Sub-Sahara Africa. Niger J Clin Pract. 2019;22:1049-54.
- [Google Scholar]
- A clinical characterization of familial keloid disease in unique African tribes reveals distinct keloid phenotypes. Plast Reconstr Surg. 2011;127:689-702.
- [CrossRef] [PubMed] [Google Scholar]






