Translate this page into:
Contemporary practice of prostate biopsy in Nigeria: Differences in technique and prophylactic measures among urologist

*Corresponding author: Friday Emeakpor Ogbetere, Department of Surgery, Edo State University, Uzairue, Edo State, Nigeria. fridayemeakpor@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ogbetere FE, Otobo OF, Akporeha HN. Contemporary practice of prostate biopsy in Nigeria: Differences in techniques and prophylactic measures among urologists. Ann Med Res Pract 2021;2:7.
Abstract
Objectives:
Prostate cancer is the most common cancer affecting men in Nigeria. Trans-rectal ultrasound-guided biopsy of the prostate is routinely performed to diagnose prostate cancer. Though safe, prostate biopsy may be associated with some complications. In Nigeria, there are scanty national guidelines on prophylactic measures and techniques in prostate biopsy. The aim of the study was to assess the pre-biopsy prophylactic measures and biopsy protocols employed by Nigerian Urologists.
Material and Methods:
A survey questionnaire was distributed during the 2019 Annual General Meeting of the Nigerian Association of Urologic Surgeons and information collected on the biopsy route, use of anesthesia, antibiotic prophylaxis, number of samples taken, and possible complications.
Results:
A total of 72 urologists participated in the study. Bowel preparation was performed by 10 (13.9%) participants for a duration of 1–3 days. All urologists used the transrectal route and anesthesia was given by all. Prophylactic antibiotics were given by all participants. Our participants administered antibiotic prophylaxis for a period of 1, 3, 5, or 7 days (4.2%, 23.6%, 43.1%, and 22.2%, respectively). Ciprofloxacin/metronidazole combination was most commonly prescribed (70.8%). Most urologists (69.4%) commonly take between 8 and 12 core tissues per biopsy session. The most common complication was hemorrhage (43.1%), followed by perineal pain (40.3%).
Conclusion:
There is a lack of evenness in pre-biopsy prophylactic measures and biopsy protocol among Nigerian Urologists. There is a need for a Nigerian guideline to elucidate the most appropriate antibiotic(s), route of administration and duration of treatment, the preferred anesthesia type, and the number of core-tissues that are appropriate.
Keywords
Prostate biopsy
Prebiopsy prophylactic measures
Prostate biopsy protocol
Prostate biopsy complications
INTRODUCTION
Prostate biopsy is the established mode of obtaining tissues for histologic diagnosis in patients with suspected prostate cancer. Although the indications have remained the same, the methods have evolved over the years.[1-3]
The first review of the complications of needle biopsy of the prostate was done by Wendel and Evans,[4] while the effectiveness of antibiotic prophylaxis in prostate biopsy was first documented by Crawford et al.[5] in 1982. Subsequently, the use of prophylactic antibiotics in transrectal prostate biopsy became the standard practice amongst urologists. However, there is no consensus among urologists regarding the type, route, timing, and duration of administration of antibiotics prophylaxis in patients undergoing transrectal needle biopsy of the prostate (TNBP).[6-8] In addition, opinions differ regarding the value of pre-biopsy enema,[9,10] the type of anesthesia[11-14] and the techniques for TNBP.[15]
In this study, we aim to evaluate the current practice of Nigerian Urologists regarding prostate biopsy techniques, the pre-biopsy prophylactic measures, and to determine the perceived most common complication following prostate biopsy.
MATERIAL AND METHODS
In this study, we developed a ten-question survey questionnaire and distributed same to Urologists practicing in Nigeria at the 2019 Annual Scientific Conference of the Nigerian Association of Urological Surgeons. The questionnaire gathered information regarding demographics, pre-biopsy patient preparation, antibiotics prophylaxis, methods of prostate biopsy, average number of core tissues, anesthesia for biopsy, and time from biopsy to obtaining results. The survey was administered on November 23, 2019, and retrieved same day.
All participants were informed about the voluntary nature of their participation and that their responses will be kept confidential. No financial compensation was given in exchange for participation.
RESULTS
Seventy-two urologists from 34 public and private hospitals in Nigeria completed the survey. Majority of the respondents (97.2%, n = 70) were from public hospitals. The years of practice range from 1 to 30 years (mean = 6.74 years). Table 1 shows the distribution of the years of practice of the participants.
| Years of practice | Frequency | Percent | Valid percent | Cumulative percent |
|---|---|---|---|---|
| 1–5 years | 38 | 52.8 | 52.8 | 52.8 |
| 6–10 years | 21 | 29.2 | 29.2 | 81.9 |
| More than 10 years | 13 | 18.1 | 18.1 | 100.0 |
| Total | 72 | 100.0 | 100.0 |
Of the 72 respondents, 10 (13.9%) do bowel preparation before prostate biopsy while 62 (86.1%) only request their patients to empty their bowel on the morning of the procedure. Of the ten urologists that do bowel preparation, five do for 1 day, four for 2 days, and one does for 3 days before biopsy.
Table 2 shows that a bulk of the participants (83.3%, n = 60) use digitally-guided TNBP, while the remaining use either transrectal ultrasound-guided (TRUS) or a combination of both. Regarding the number of core tissues per biopsy, most urologists (76.3%) employ extended biopsy protocol with 69.4% of these obtaining between 8 and 12 core tissues while 6.9% obtain more than 12 core tissues on the average. A handful (23.6%) still practices sextant biopsy protocol. There was, however, a variation among the urologists within the same hospital in terms of the number of core tissues obtained per session. Majority (68%) of urologists use either topical anesthesia (with lignocaine gel) or caudal block. Twenty-six percent of the urologists use a combination of both lignocaine gel and caudal block. Figure 1 depicts the various pre-biopsy anesthesia used by the study participants.
| Methods of biopsy | Frequency | Percent | Valid Percent | Cumulative Percent |
|---|---|---|---|---|
| Digital-guided | 60 | 83.3 | 83.3 | 83.3 |
| TRUS-guided | 8 | 11.1 | 11.1 | 94.4 |
| Digital/TRUS-guided | 4 | 5.6 | 5.6 | 100.0 |
| Total | 72 | 100.0 | 100.0 |
TRUS: Trans-rectal ultrasound-guided
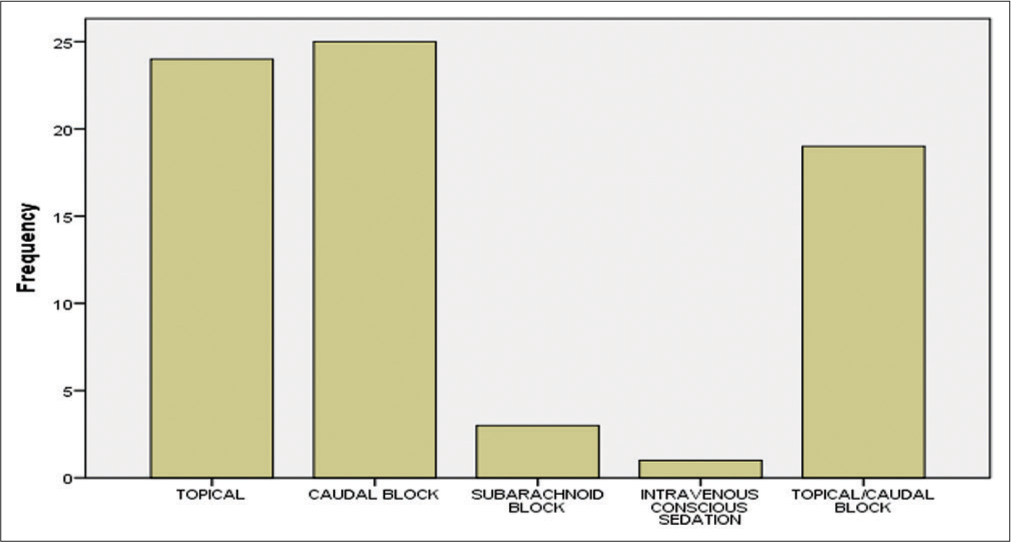
- Types of anesthesia used by the respondents.
There was a wide inter-hospital variation in antibiotic choice, routes of administration [Figure 2], combinations, duration, and time of administration.
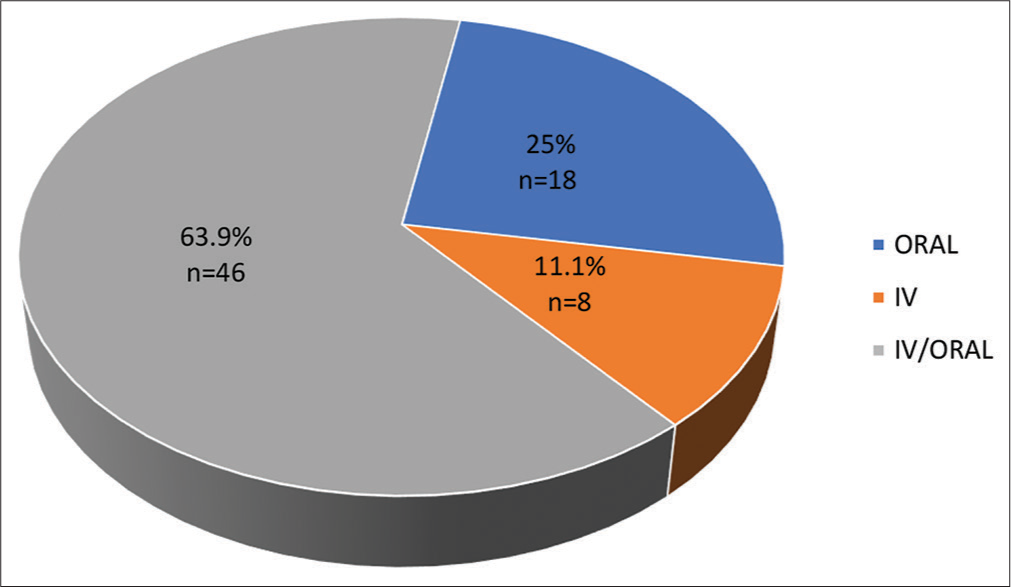
- Routes of antibiotics administration.
Regarding the time of commencement of antibiotics [Table 3], one of the participants did not respond. Of the 71 urologists that responded to this question, 57 (79.2%) give about 1 h before the commencement of the procedure.
| Antibiotics commencement time | Frequency | Percent | Valid percent | Cumulative percent |
|---|---|---|---|---|
| 3 days before TNBP | 6 | 8.3 | 8.5 | 8.5 |
| 1 day before TNBP | 5 | 6.9 | 7.0 | 15.5 |
| 2–3 h before TNBP | 3 | 4.2 | 4.2 | 19.7 |
| 1 h before TNBP | 57 | 79.2 | 80.3 | 100.0 |
| Total response | 71 | 98.6 | 100.0 | |
| No response | 1 | 1.4 | ||
| Total | 72 | 100.0 |
TNBP: Transrectal needle biopsy of the prostate
Five different antibiotic regimens with two major antibiotics combinations were recorded. The antibiotics most frequently used were the fluoroquinolones/metronidazole combination (70.8%, n = 51) [Table 4].
| Antibiotics combinations | Frequency | Percent | Valid Percent | Cumulative Percent |
|---|---|---|---|---|
| Quinolones/metronidazole | 51 | 70.8 | 70.8 | 70.8 |
| Cephalosporins/metronidazole | 14 | 19.4 | 19.4 | 90.3 |
| Gentamicin/metronidazole | 1 | 1.4 | 1.4 | 91.7 |
| Others | 6 | 8.3 | 8.3 | 100.0 |
| Total | 72 | 100.0 | 100.0 |
TNBP: Transrectal needle biopsy of the prostate
The duration of antibiotics prophylaxis ranged from a single pre-biopsy dose to a 5-day extended prophylaxis with most hospitals (59.4%) giving a single dose an hour before the procedure [Figure 3]Table 5 shows the participant’s response regarding the most common complication following prostate biopsy in their practice.
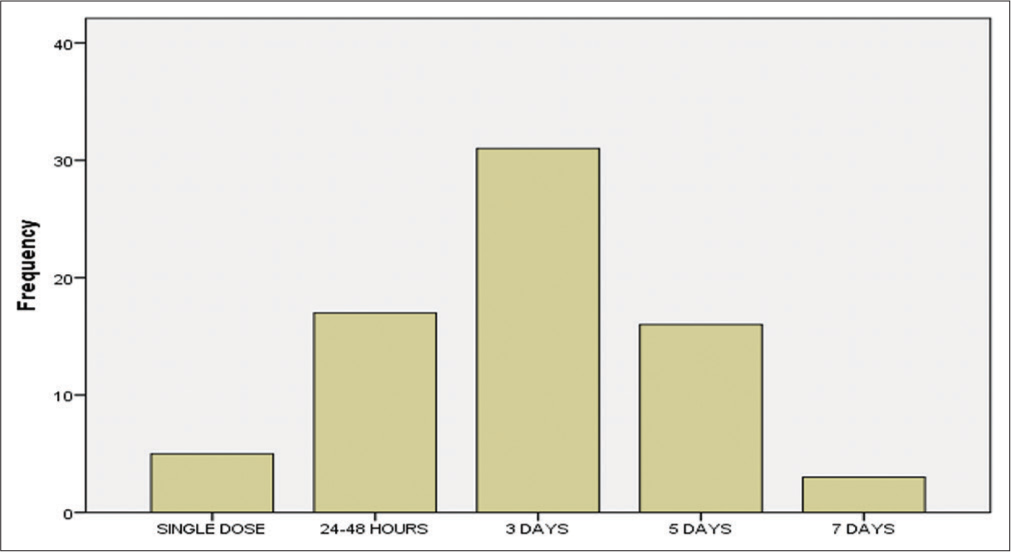
- Duration of antibiotics prophylaxics.
| Complications | Frequency | Percent | Valid percent | Cumulative percent |
|---|---|---|---|---|
| Perineal Pain | 29 | 40.3 | 40.3 | 40.3 |
| Hemorrhage | 31 | 43.1 | 43.1 | 83.3 |
| Fever | 10 | 13.9 | 13.9 | 97.2 |
| AUR | 2 | 2.8 | 2.8 | 100.0 |
| Total | 72 | 100.0 | 100.0 |
TNBP: Transrectal needle biopsy of the prostate
Concerning the duration between biopsy procedure and obtaining histology report, most urologist (88.8%) said they obtain their histological results between 2 and 3 weeks. A few (7%), however, who practice in remote parts of the country required about 4–5 weeks to get histology results while three of the respondents get the histology report in about 1 week.
DISCUSSION
Prostate biopsy is a common procedure performed by urologists worldwide. Despite guidelines to ensure uniformity, dissimilarities still exist between centers and even among urologists within the same hospital globally.[15] This research showed a wide variability in pre-procedural measures and techniques among Nigerian Urologists.
TRUS biopsy is currently the gold standard in obtaining tissues for histology.[3,6,7] All urologists in this study use the trans-rectal approach. Another route of biopsy includes trans-perineal which is presently out of favor.[3]
Different biopsy protocols have been used for prostate biopsy. These include the sextant, extended, and the saturation biopsy protocols.
This work showed that extended biopsy protocol with 8–12 cores per biopsy session was most routinely used by urologists (76.3%), which was in line with the guidelines at that moment.[16] Sextant biopsy is no longer considered adequate. At the moment, 8–12 core biopsies are recommended[17] with more than 12 cores not being significantly more conclusive.[18]
Random systematic TRUS prostate biopsy of the prostate is presently the preferred method.[19] The European Association of Urology[20] in recent times recommended performing multi-parametric magnetic resonance imaging (mpMRI) before prostate biopsy in biopsy-naïve patients. Other recommendations include MRI guided or MRI/ TRUS fusion guided prostate biopsy.[20] However, in the sub-Saharan Africa, due to limited resources and economic challenges, digitally-guided transrectal prostate biopsy is still predominantly practiced. In our survey, only a few centers (16.7%) located majorly in the urban areas perform TRUS-guided biopsy while the majority (83.3%) use digital guidance.
Various pharmacological regimens have been used for pain control following prostate biopsy. These include topical anesthetic agents such as lidocaine gel and lidocaine-prilocaine cream, regional anesthesia such as periprostatic nerve block and the less often used general anesthesia.[12-14] In this study, most participants use caudal block, or a combination of caudal block and topical anesthesia. The high patronage of topical or caudal anesthesia may be due to the non-availability of TRUS scan in most centers in Nigeria.
The use of prophylactic antibiotics plays an important role in reducing post-procedural fever and urinary tract infection (UTI) following prostate biopsy.[21] However, drug choice and treatment courses are variable in different Nigerian hospitals. Variation in antibiotic choice could be related to a lack of strong evidence, with resultant inconsistent and unclear recommendations in urological guidelines. While these guidelines generally recommend antimicrobial prophylaxis in trans-rectal prostate biopsy, the choice of regimen, duration, and the starting moment is ambiguous.[18-20] Sabbagh et al.[22] suggested that a single-dose regimen of the combination of fluoroquinolones and nitroimidazoles is as effective as 3 days of treatment of same combination. According to the current guidelines, the length of antimicrobial prophylaxis should be limited to about 24 h.[19,20] In this study, only about 7% of the Urologists give antibiotics for only 24 h with most giving antimicrobial prophylaxis for 3–7 days. The reason for this discrepancy could be due to lack of standardized guidelines for prophylaxis in TNBP. This same reason could account for the variability and diversity in antibiotics combination and commencement time noted in this study.
The most common urological complications of TNBP are hemorrhage (which include hematuria, rectal bleeding, and hematospermia), perineal pain, UTI, acute urinary retention, erectile dysfunction, and vasovagal response.[15,16] Regarding hemorrhage, recent data suggest that hematuria is noted in 23–84%, rectal bleeding in 17–45%, and hematospermia in 12–93% of men post-TNBP.[23] The most common complication noted in this study was hemorrhage and closely followed by perineal pain. This finding mirrors the reports of many researchers who reported hemorrhagic complications as the most common in TNBP.[7,8,24]
CONCLUSION
This study shows that the lack of standardized, harmonized, and clear guidelines in prebiopsy prophylactic measures may lead to discrepancy in the quality of prostate biopsy services offered by the urologists, which means some patients may be better taken care of in some health facilities than the others. The heterogeneity of the reported prophylactic measures is probably due to poor evidence. Therefore, there is a need for well thought-out, adequately powered trials of excellent design with respect to pre-biopsy prophylactic regimens. These high-quality researches will give rise to evidence-based, distinct guidelines and offers urologists better guidance with respect to prebiopsy prophylactic measures.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Young's Practice of Urology. Vol 2. (1st ed). Philadelphia, PA: WB Saunders; 1926. p. :414-512.
- [Google Scholar]
- Diagnostic application of ultrasonotomography to the prostate. Nihon Hinyokika Gakkai Zasshi. 1968;59:273-9.
- [CrossRef] [PubMed] [Google Scholar]
- Random systematic versus directed ultrasound guided transrectal core biopsies of the prostate. J Urol. 1989;142:71-5.
- [CrossRef] [Google Scholar]
- Complications of punch biopsy of the prostate gland. J Urol. 1967;97:122-6.
- [CrossRef] [Google Scholar]
- Prevention of urinary tract infection and sepsis following transrectal prostatic biopsy. J Urol. 1982;127:449-51.
- [CrossRef] [Google Scholar]
- Antibiotic prophylaxis for transrectal needle biopsy of the prostate: A randomized controlled study. BJU Int. 2000;85:682-5.
- [CrossRef] [PubMed] [Google Scholar]
- Single-dose oral ciprofloxacin versus placebo for prophylaxis during transrectal prostate biopsy. Urology. 1998;52:552-8.
- [CrossRef] [Google Scholar]
- Antibiotic prophylaxis in prostate biopsy. A comparative randomized clinical assay between ciprofloxacin, norfloxacin and chloramphenicol. Int Braz J Urol. 2003;29:313-9.
- [CrossRef] [PubMed] [Google Scholar]
- Bisacodyl rectal preparation can decrease infectious complications of transrectal ultrasound-guided prostate biopsy. Urology. 2003;62:461-6.
- [CrossRef] [Google Scholar]
- Transrectal ultrasound guided biopsy of the prostate. Do enemas decrease clinically significant complications? J Urol. 2001;166:82-5.
- [CrossRef] [Google Scholar]
- Patients' tolerance of transrectal ultrasound-guided prostatic biopsy: An audit of 104 cases. BJU Int. 1999;83:792-5.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of prostate biopsy on patient well-being: A prospective study of pain, anxiety and erectile dysfunction. J Urol. 2001;165:445-54.
- [CrossRef] [PubMed] [Google Scholar]
- Transrectal ultrasound guided prostatic nerve blockade eases systematic needle biopsy of the prostate. J Urol. 1996;155:607-9.
- [CrossRef] [Google Scholar]
- A randomized prospective trial of intrarectal lidocaine for pain control during transrectal prostate biopsy: The Emory University experience. J Urol. 2000;164:397-9.
- [CrossRef] [PubMed] [Google Scholar]
- Current practice of prostate biopsy in Australia and New Zealand: A survey. Urol Ann. 2015;7:315-9.
- [CrossRef] [PubMed] [Google Scholar]
- Prostate testing for cancer and treatment (ProtecT) feasibility study. Health Technol Assess. 2003;7:1-88.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic value of systematic biopsy methods in the investigation of prostate cancer: A systematic review. J Urol. 2006;175:1605-12.
- [CrossRef] [Google Scholar]
- Prostate biopsy techniques and pre-biopsy prophylactic measures: Variation in current practice patterns in the Netherlands. BMC Urol. 2020;20:24.
- [CrossRef] [PubMed] [Google Scholar]
- A multi-center, controlled, randomized, open-label clinical study of levofloxacin for preventing infection during the perioperative period of ultrasound-guided transrectal prostate biopsy. Eur J Clin Microbiol Infect Dis. 2016;35:1877-81.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective randomized trial of 1-day versus 3-day antibiotic prophylaxis for transrectal ultrasound guided prostate biopsy. Can J Urol. 2004;11:2216-9.
- [Google Scholar]
- Optimization of prostate biopsy: Review of technique and complications. Urol Clin North Am. 2014;41:299-313.
- [CrossRef] [PubMed] [Google Scholar]
- Rates and determinants of complications following trans-rectal prostate biopsy in Enugu, Nigeria. J Adv Med Med Res. 2017;23:1-8.
- [CrossRef] [Google Scholar]






