Translate this page into:
Comparison of low dose vaginal misoprostol with Foley catheter balloon as preinduction cervical ripening agents in term pregnancies

*Corresponding author: Dr. Dalyop Davou Nyango, Department of Obstetrics and Gynaecology, Jos University Teaching Hospital, Plateau, Nigeria. drnyango@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Nyango DD, Daloek M, Kahansim ML. Comparison of low dose vaginal misoprostol with Foley catheter balloon as preinduction cervical ripening agents in term pregnancies. Ann Med Res Pract 2020;1:10.
Abstract
Objective:
One of the obstetricians’ nightmare is managing high-risk pregnancies. Also, the emerging trend by pregnant women requesting for specific delivery dates for social reasons adds to this burden. In both instances, the obstetrician is faced with the challenge of inducing labor where the cervix is still unfavorable. The objective of the study was to compare the effectiveness of loe dose vaginal misoprostol and transcervical extra-amniotic Foley catheter balloon as pre-induction cervical ripening agents in term pregnancies.
Material and Methods:
This was a prospective, single-blind, randomized comparative trial at a tertiary hospital. Pregnant women at term in whom induction of labor was indicated, who made the inclusion criteria and who gave their consent were randomly assigned to either the vaginal misoprostol or the Foley catheter balloon group. Oxytocin was used for the augmentation of labor subsequent to the artificial rupture of the membranes according to the departmental protocols.
Results:
One hundred and fifty women were recruited and randomized (75 in each group). In the misoprostol group, 58 (77.3%) women achieved cervical ripening (cervical dilation of ≥4) within 12 h, compared to 43 (57.3%) in the Foley catheter balloon group. Spontaneous vaginal delivery within 12 h was 88.0% and 66.3% in the misoprostol and Foley catheter group, respectively. However, 34.7% in misoprostol group had precipitate labor (induction-to-delivery interval ≤3 h), while 9.3% in the Foley catheter group had prolonged labor. There were no significant differences in the incidence of meconium staining and 1st min Apgar scores of the babies in the two groups.
Conclusion:
Low dose (25 μg) vaginal misoprostol is a more effective pre-induction cervical ripening agent compared to the conventional transcervical extra-amniotic Foley catheter balloon method. While uterine hyperstimulation is the major risk in the misoprostol group, long induction-to-delivery interval is associated with labors induced following use of Foley catheter balloon as the pre-induction cervical ripening agent.
Keywords
Vaginal misoprostol
Unfavorable cervix
Cervical ripening
Induction of labor
Foley catheter balloon
INTRODUCTION
Globally, one of the obstetricians’ nightmares is managing high-risk pregnancies, i.e., pregnancies in which the risks of waiting for the onset of spontaneous labor are judged to be greater than the risks associated with shortening the duration of the pregnancy. These circumstances include the gestational age of 41 completed weeks or more, hypertensive disorders, maternal medical complications, fetal death, fetal growth restriction, and chorioamnionitis. Furthermore, there is an emerging trend among pregnant women requesting obstetrician to shorten the duration of their pregnancies for social reasons and/or occasionally health-care workers convenience.[1,2] Induction of labor is the frequently used method of terminating pregnancy in both instances. However, the obstetrician is usually confronted with an unfavorable cervix. An unfavorable cervix is a critical factor the obstetrician must overcome to improve the efficacy of induction of labor. At present, both medical and mechanical methods have been applied for cervical ripening in women with an unfavorable cervix.[3] The Foley catheter balloon is one of the oldest mechanical devices commonly used for cervical ripening and induction of labor. Inserted transcervically into the extra-amniotic space, it acts not only as a mechanical dilator of the cervix but also has the added advantage of stimulating the release of endogenous prostaglandins from the fetal membranes. Foley catheters achieved similar vaginal delivery rates, with fewer maternal, and neonatal side effects.[4] However, controversies among practitioners continue to trail its use as an effective pre-induction cervical ripening agent. While some argue about the time limitation for exposure to extra-amniotic balloon (i.e., Waiting for spontaneous expulsion or setting a maximum time limit),[5,6] others argue about the volume of fluid used to inflate the balloon.[7,8] Even the recently introduced double-balloon catheter for cervical ripening and labor induction has not demonstrated any superiority.[9] The hygroscopic and osmotic dilators are another group of effective mechanical dilators. However, they are associated with an increased risk of maternal infection and, therefore, seldom use in the induction of labor at term.[10]
Prostaglandins are now widely used in obstetrics practice to improve the efficacy of cervical ripening and induction of labor.[11] Several studies have shown that prostaglandins are superior to the Foley catheter balloon.[12-14] Importantly, vaginal prostaglandins are more cost-effective compared to the transcervical extra-amniotic Foley catheter balloon.[15] Misoprostol (Cytotec, Searle) is a prostaglandin E1 analog that is equally effective and with minimal systemic side effects when administered vaginally.[16,17] Importantly, it is particularly useful in low-resource settings as it is less expensive and also stable at room temperature within its packaging in comparison with the widely used prostaglandins E2. Various regimens of vaginal misoprostol have been advocated. The current consensus is the use of 25 μg every 3–6 h.[18] Higher doses have been associated with uterine rupture and significantly higher cesarean section rate caused by abnormal fetal heart rate patterns compared with 25 µg dose.[16,19]
The aim of this study is to compare the effectiveness of low dose (25 µg) vaginal misoprostol and transcervical extra- amniotic Foley catheter balloon as pre-induction cervical ripening agents in term pregnancies.
MATERIAL AND METHODS
The study was approved by the ethical committee of Jos University Teaching Hospital. The study was explained to all the subjects, and each woman gave written informed consent to participate in this study.
Study design
This was a prospective single-blind, and randomized comparative trial.
Setting
The data were collected in Jos University Teaching Hospital, which is a tertiary hospital, between February 1, 2013, and April 30, 2014.
Subjects
Women scheduled for induction of labor who had unfavorable cervix and who met the inclusion criteria for the study were screened for eligibility. Inclusion criteria were gestational age ≥37 weeks; singleton pregnancy with cephalic presentation; intact membranes; reactive non-stress test; and Bishop’s score <6. Women gave a written consent. Women with vaginal infection, antepartum bleeding, placenta praevia, intrauterine fetal death, women with immunosuppression, previous uterine scar, women whose fetal membranes are already ruptured, refusal to give consent or women with suspected fetal macrosomia or any other contraindication to vaginal delivery were excluded from the study.
Sample size determination
The sample size in this study was calculated using the formula for comparing two groups (paired design).[20] In this formula, P1 and P2 represent the prevalence of induction of labor using misoprostol[21] and using transcervical Foley catheter,[22] respectively. Both representing prevalence from similar studies in comparable populations as recommended.[23] Using this formula, the minimum sample size for the study was 56. However, we recruited 75 women with the assumption that a proportion of eligible women may refuse to participate or drop out before the end of the study. The assumption is that using this formula will give us a power of 80% or higher (P < 5%) if really there is an important difference between the two groups.
Randomization
The sequence of computer-generated numbers was placed into numbered opaque envelopes by an uninvolved third party before the initiation of the study. Each participant was assigned to the vaginal misoprostol or the Foley catheter balloon group by drawing the next in a series of opaque sealed envelopes that had been generated from a random number table.
Intervention
Before the study started, the researchers acquaint themselves with the standard operative protocol and Bishop scoring system. Women who made the inclusion criteria and gave their consent were randomly assigned to either the vaginal misoprostol or the Foley catheter balloon group. We then recorded medical history and reviewed the indication for induction and explained the objectives of the study to the pregnant women. The gestational age was calculated using last menstrual period (LMP) if the woman keep’s a menstrual calendar. Where the woman was sure of her LMP but does not keep a menstrual calendar, the LMP was used if ultrasound’s results were in agreement with that estimated by LMP within 7 days up to 19 weeks 6 days, within 14 days at 20–29 weeks 6 days, or within 21 days at 30 weeks or beyond. If LMP data were not available, dating was based on the first ultrasound scan. The status of the cervix was determined by the standardized method of semi-quantitative clinical scoring of the cervix, as described by Bishop in 1964.[24] An obstetrics ultrasound scan and cardiotocogram were also performed before the administration of either intervention. If the cervical score was <6, with reactive cardiotocogram, the woman was randomly assigned by opening the consecutively numbered envelope to receive either vaginal misoprostol 25 µg four hourly (to a maximum of three doses) placed digitally in the posterior vaginal fornix or a size 16 Foley catheter was passed transcervically into the extra-amniotic space under aseptic technique and the balloon inflated with 40 ml sterile water for a maximum of 24 h.
Patients were transferred to the labor ward for oxytocin infusion and synchronous amniotomy. Labor was strictly monitored by the use of partograph. Women with any abnormality of the fetal heart rate, uterine hyperstimulation or with a Bishop score of <6 excluded from the study. These procedures were carried out by the researcher alone to remove the subjectivity associated with the assessment.
Outcome measures
The primary outcome measure is cervical dilatation of 4 cm and induction-delivery interval. Secondary outcomes included uterine hyperstimulation, mode of delivery, the evidence of fetal distress in labor, Apgar scores at 1 and 5 min.
Technique for placement of Foley’s catheter balloon
The procedure was carried out between 4 and 6 pm. With the patient in the dorsal position, the vulva and vagina were cleansed with an antiseptic solution of Savlon. The cervix was exposed with a sterile Grave’s speculum and cleansed with a Savlon antiseptic solution. A 16-F Foley catheter was introduced through the vagina into the endocervical canal under direct visualization. Once the catheter has past the internal operating system (OS) into the potential space between the amniotic membrane and the lower uterine segment, the balloon was inflated with 40 mL of sterile water or normal saline solution and the balloon pulled so that it rests against the internal OS of the cervix. The external end of Foley catheter was strapped under moderate tension to the medial aspect of the woman’s thigh. Non-stress test was conducted after catheter insertion. Instruction was left to inform the researchers if the catheter falls, woman draining liquor, or contractions start. When the catheter falls or in the absence of any of the above, at 6 am vaginal examination is done to re-assess the favorability of the cervix and induction of labor is commenced. When the Foley catheter falls off, or if the Bishop score was six or more, the patient was transferred to the labor ward for oxytocin infusion and synchronous artificial rupture of the membranes. In this study, we define “ripening time” as the maximum time limit for Foley catheter balloon exposure. In all groups, the Foley catheter was removed for the following reasons: (1) The time limit for ripening was reached; (2) spontaneous rupture of membranes occurred; (3) the balloon was expelled spontaneously; (4) women entered the active phase of labor; or (5) hyperstimulation or fetal distress was suspected. However, if none of these occurs, catheter is removed at 6 am and Bishop scoring repeated. If the Bishop score is <6 after 12 h, the catheter will be reinserted.
Technique for application of vaginal misoprostol (Cytotec) tablets
With the patient in dorsal position, the vulva and vagina were cleansed with antiseptic solution of Savlon. The 25 µg misoprostol tablet was placed between the tips of the index and middle fingers of sterile gloved hand. The fingers were gently introduced into the vagina to the level of the posterior fornix. The fingers were then open to drop the tablet and were gently withdrawn, ensuring the tablet remains in place. The woman is asked to turn to her left side for few minutes before leaving the couch. Four hours later, the procedure is repeated. Abdominal examination and cervical assessment were carried out before the insertion of the next dose of misoprostol. No further doses of misoprostol were given if there were uterine contractions, if membranes ruptured spontaneously or if there were any fetal heart rate abnormalities.
Technique for performing amniotomy
Amniotomy was done at the commencement of the oxytocin infusion. A pelvic examination is performed to evaluate the cervix and station of the presenting part. The presenting part was checked to ensure it had descended. The fetal heart rate is recorded before and after the procedure. A pair of Kocher’s forceps was inserted through the cervical OS, guided by the index and middle fingers of the examination hand, by sliding it along the fingers until it touches the fetal head, it was then open and carefully grasp the fetal membranes. Gentle traction was applied to stretch the membranes and the examining fingers used to confirm. The membranes were then ruptured by applying additional traction on the Kocher’s forceps. The fingers were left in the vaginal for few minutes to regulate the flow of the liquor. The nature of the amniotic fluid is recorded.
Technique for intravenous oxytocin infusion
The induction procedure was carried out in labor ward. The criteria for the onset of labor were painful contractions accompanied by effacement of at least 80%. The active phase was defined as complete cervical effacement and dilatation of at least 4 cm. For women who did not enter spontaneous labor during the ripening process, synchronous amniotomy was preformed once the catheter was expelled or removed, in the case of misoprostol, when the cervix is 4 cm dilated. Induction of labor was done with the use of 5 IU oxytocin in 500 ml of 5% dextrose water administered intravenously using I.V giving set starting at 10 drops/min. The dose was escalated by 10 drops/min to a maximum of 60 drops/min or when adequate uterine contractions, defined as 3–4 contractions in 1 min lasting 40–45 s are achieved. Augmentation of labor was commenced with intravenous oxytocin if the contraction frequency was unsatisfactory (<3 contractions/10 min). Oxytocin was discontinued once the women were deemed to be in active labor. When a woman was in active labor, maternal pulse rate, blood pressure, and temperature were recorded every hour. While uterine contractions and vaginal examination were recorded every 4 h, fetal heart rate was recorded quarter-hourly on the partograph.
Hyperstimulation was defined as 6 or more uterine contractions in every 10 min in a consecutive 30-min interval with or without fetal heart rate changes. Failed induction was defined as a failure to progress into the active phase of labor, despite the maximum 60 dpm of oxytocin over 24 h after amniotomy. Failure to progress was diagnosed as unchanged cervical dilation in a 4-h interval, despite adequate uterine contraction. Chorioamnionitis was diagnosed as maternal fever (≥38°C), accompanied by maternal tachycardia (>100 bpm), or uterine fundal tenderness, or fetal tachycardia (>160 bpm), or purulent amniotic fluid. PPH was defined as a blood loss of more than 500 mL within 24 h of delivery. Blood loss was measured by: (1) Collecting and recording of blood in bedpan containers, and (2) weighing of materials including soaked sponges and pads on a scale and subtracting the known dry weights of these materials.
Data collection/data analysis/statistical method
Data analysis was conducted using the Epi info 3.5.2 statistical software. Categorical outcomes were summarized using frequency distributions. Normally distributed data were presented as mean with SD. Chi-square analysis was used for comparing proportions of categorical variables while the student’s test was used for comparing means of continuous variables where applicable. For categorical data, we calculated that P < 0.05 was taken as being statistical significance methods.
RESULTS
During the study period, 168 women were screened for eligibility. Seven women declined to participate in the study, 8 and 2 were considered inappropriate for induction of labor because the presenting part was not engaged and for suspected low lying placenta, respectively. Thus, 150 women were recruited and randomized (75 in each group). The mean age of the participants was 31.28 ± 5.09 years for the misoprostol and 30.16 ± 7.14 years for the Foley’s catheter respondents. The indication for induction of labor, mean gestational age, and Bishop Score before cervical ripening was comparable in both groups [Table 1]. The major indications for induction of labor were prolonged pregnancies and hypertensive disorders [Figure 1]. In the misoprostol group, 58 (77.3%) women achieved cervical ripening (cervical dilation of ≥4) within 12 h, compared to 43 (57.3%) in the Foley catheter balloon group. In the catheter group, eight women had the catheter removed on gentle traction, while five women their catheter balloon delayed for about 24 h.
Spontaneous vaginal delivery within 12 h was 88.0% and 66.3% in the misoprostol and Foley catheter group, respectively. However, 34.7% in misoprostol group had precipitate labor (induction delivery interval ≤3 h), while 9.3% in the Foley catheter group had prolonged labor [Figure 2]. The indication for cesarean section in the misoprostol group was due to suspected fetal distress in first stage of labor, while in the Foley catheter balloon group, failure to progress due to cephalopelvic disproportion and suspected chorioamnionitis were the main indications.
There were no significant differences in the incidence of meconium staining and 1st min Apgar scores of the babies in the two groups: Foley’s catheter balloon and misoprostol groups. However, six babies had Apgar scores of <7 in the misoprostol group in the 5th min, though they did not require any intervention [Table 2].
| Characteristics | Misoprostol group | Foley catheter balloon group | Mean |
|---|---|---|---|
| Maternal age (years; mean±SD) | 31.28±5.09 | 30.16±7.14 | 30.72±6.20 |
| Parity n(%) | |||
| 0 | 49 (65.3) | 43 (57.3) | 46 (61.3) |
| 1–4 | 20 (26.7) | 22 (29.3) | 21 (28.0) |
| ≥5 | 6 (8.0) | 10 (13.3) | 8 (10.7) |
| Educational status | |||
| Primary | 6 (8.0) | 12 (16.0) | 18 (12.0) |
| Secondary | 35 (46.7) | 29 (38.7) | 64 (42.7) |
| Tertiary | 34 (45.3) | 34 (45.3) | 68 (45.3) |
| GA (mean±SD) | 39.41±2.48 | 39.11±1.71 | 39.26±2.13 |
| Bishop score (<6) | 75 | 75 |
| Outcome | Foley’s catheter F (%) | Misoprostol F (%) | χ2 | Df | P-value | |
|---|---|---|---|---|---|---|
| Apgar scores 1st min | <7 ≥7 Total |
18 (24.0) 57 (76.0) 75 (100.0) |
19 (25.3) 56 (74.7) 75 (100.0) |
0.036 | 1 | 0.850 |
| Apgar scores 5th min | <7 ≥7 Total |
0 (0.0) 75 (100.0) 75 (100.0) |
6 (8.0) 69 (92.0) 75 (100.0) |
4.340 | 1 | 0.037 |
| Birth weight (kg) | 2–2.9 3–3.9 ≥4.0 Total |
26 (34.7) 41 (54.7) 8 (10.7) 75 (100.0) |
23 (30.7) 52 (69.3) 0 75 (100.0) |
0.621 | 2 | 0.733 |
| Meconium stained liquor | Yes No Total |
23 (30.7) 52 (69.3) 75 (100.0) |
15 (20.0) 60 (80.0) 75 (100.0) |
2.256 | 1 | 0.133 |
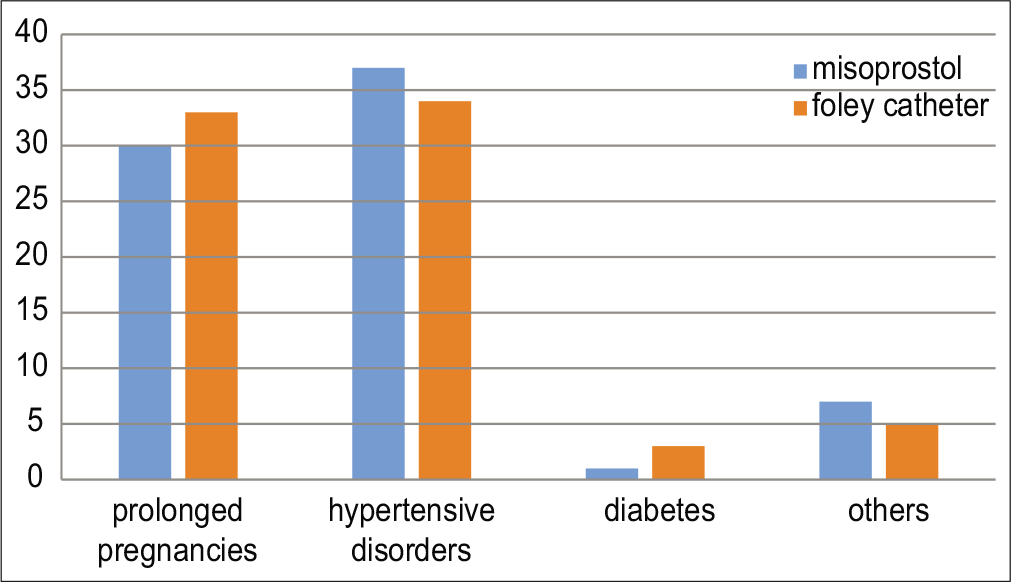
- Indications for induction of labour.

- Induction to delivery interval.
DISCUSSION
The result of our study shows that low dose (25 µg) vaginal misoprostol is a more effective cervical ripening agent than the conventional transcervical extra-amniotic Foley catheter balloon method. Fifty-eight (77.3%) of women achieved cervical ripening (cervical dilation of ≥4) within 12 h in the misoprostol group, compared to 43 (57.3%) in the catheter balloon group. This is statistically significant (P = 0.001). Furthermore, induction to delivery interval was shorter in the misoprostol group, with 88.0% spontaneous vaginal delivery within 12 h compared to 66.6% in the Foley catheter group [Figure 2]. This is similar to the previous studies.[4,25] The overall spontaneous vaginal delivery rate of 66.6% and 88.0% in our study is higher than the range of 48–66% previously reported.[10,21] The type of prostaglandin used may contribute to the observed differences. These studies used prostaglandin E2 while our study used prostaglandin E1 analog. A significant finding in our study is that a high percentage (34.7%) of the women had precipitate labor and uterine hyper-stimulation 8 (10.7%) in the misoprostol group as compared with 9.3% and none in the Foley catheter balloon group, respectively, even though the same oxytocin regimen was used. This may indicate that the manual method of assessing uterine contraction used may be inaccurate or the technique of digital insertion of prostaglandin tablets was not good enough. This calls for the use of the more sensitive electronic method of monitoring uterine and fetal heart rate activity for patients on induction of labor following cervical ripening with misoprostol. This agrees with the previous reports showing that misoprostol is associated with risk of uterine hyperstimulation which increase with higher dosage.[18,19,26] Sixteen (21.3%) of the women in the catheter balloon group had an induction to delivery interval of ≥12 h [Figure 2]. This agrees with the previous findings, which showed that induction of labor following the use of transcervical extra- amniotic Foley catheter as the cervical ripening agent is associated with longer labor ward stay and higher costs due to longer induction to delivery interval.[13,15] This is particularly worrisome for the developing economy where cost of services is of great concern. In addition to the fact that some patients had the duration of their catheter extended from 12 to 24 h, shows that Foley catheter balloon, which dilates the cervix mechanically, is associated with a delayed transition to active labor. Therefore, our study also suggest that longer period of stay of the Foley catheter balloon may reduce the problem of longer induction to delivery interval since studies have shown that the Foley catheter balloon is safe for up to 24 h provided that the membranes are intact and the fetomaternal conditions remain satisfactory.[5]
The cesarean section rate in our study was 6.7% in the misoprostol group. This is lower than the 19.1% and 18.9% reported from systematic review of five high-quality randomized controlled trials.[22] This wide difference is expected since unlike in our study, the studies included in the systematic review used the more objective electronic fetal monitoring that is more sensitive in picking fetal heart rate pattern abnormalities and uterine hyper stimulation. Fortunately, we did not experience cases of clinical chorioamnionitis. This suggest that the 12 h is safe, although it has been reported that catheter balloon is safe for up to 24 h provided that the membranes are intact and the fetomaternal conditions remain satisfactory.[5]
There were no significant adverse neonatal outcomes in both groups we studied [Table 2]. The 1st and 5th min Apgar scores in both groups were not statistically significant (P = 0.037). Furthermore, there was no significant difference in terms of meconium staining of the liquor. These findings are similar to the previous reports.[16,22] The study had some limitations. First, this is a hospital-based study and therefore the result may not reflect the findings in the general population. Second, the study used manual method of fetal heart rate monitoring and timing of uterine contraction and therefore less objective in detecting fetal rate abnormalities and hyperstimulation. Third, lack of performing cardiotocography before insertion of additional doses of misoprostol tablets may contribute to the fetal heart rate abnormalities observed. We think that the risk of hyperstimulation leading to precipitate labor or abnormal fetal heart rate patterns can be reduced using an electronic method of assessment.
CONCLUSION
Low dose (25 µg) vaginal misoprostol is a more effective pre-induction cervical ripening agent compared to the conventional transcervical extra-amniotic Foley catheter balloon method. However, low dose vaginal misoprostol is associated with increased risk of fetal heart rate abnormalities and precipitate labor due to uterine hyperstimulation. Use of Foley catheter balloon as cervical ripening agent is associated with long induction to delivery interval with its attending risk of chorioamnionitis and cost of long labor ward stay. Therefore, our study suggests that vaginal misoprostol is a promising pre- induction cervical ripening and induction of labor agent in low- resource settings since it is equally stable at room temperature.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Indications for induction of labour: A best-evidence review. BJOG. 2009;116:626-36.
- [CrossRef] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence: Guidance, Induction of Labour In: National Collaborating Centre for Women's and Children's Health. London: RCOG Press; 2008.
- [Google Scholar]
- Labor Induction and Cervical Ripening. 2005. Available from: https://www.aafp.org/x21472.xml [Last accessed on 2005 Nov 18]
- [Google Scholar]
- Foley catheter versus vaginal prostaglandin E2 gel for induction of labour at term (PROBAAT trial): An open-label, randomised controlled trial. Lancet. 2011;378:2095-103.
- [CrossRef] [Google Scholar]
- Cervical ripening: How long can the foley catheter safely remain in the cervical canal? Afr J Reprod Health. 2002;6:98-102.
- [CrossRef] [PubMed] [Google Scholar]
- Foley catheter for induction of labor at term: An open-label, randomized controlled trial. PLoS One. 2015;10:e0136856.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized trial comparing a 30-ml and an 80-ml Foley catheter balloon for preinduction cervical ripening. Am J Obstet Gynecol. 2004;191:1632-6.
- [CrossRef] [PubMed] [Google Scholar]
- Labor induction with a foley balloon inflated to 30 ml compared with 60 ml. Obstet Gynecol. 2010;115:1239-45.
- [CrossRef] [PubMed] [Google Scholar]
- Induction of labour in nulliparous women with an unfavourable cervix: A randomised controlled trial comparing double and single balloon catheters and PGE2 gel. BJOG. 2009;116:1443-52.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanical methods for induction of labour. Cochrane Database Syst Rev. 2012;14:CD001233.
- [CrossRef] [PubMed] [Google Scholar]
- Intravaginal misoprostol as a cervical ripening agent. Br J Obstet Gynaecol. 1993;100:641-4.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized trial of preinduction cervical ripening: Dinoprostone vaginal insert versus double-balloon catheter. Am J Obstet Gynecol. 2012;207:125.e1-7.
- [CrossRef] [PubMed] [Google Scholar]
- Is transcervical Foley catheter actually slower than prostaglandins in ripening the cervix? A randomized study. Am J Obstet Gynecol. 2011;204:338.e1-7.
- [CrossRef] [PubMed] [Google Scholar]
- A randomised controlled trial of intravaginal dinoprostone, intravaginal misoprostol and transcervical balloon catheter for labour induction. BJOG. 2008;115:1443-50.
- [CrossRef] [PubMed] [Google Scholar]
- Cost-effectiveness of induction of labour at term with a Foley catheter compared to vaginal prostaglandin E2 gel (PROBAAT trial) BJOG. 2013;120:987-95.
- [CrossRef] [PubMed] [Google Scholar]
- Misoprostol administered vaginally for cervical ripening and labour induction in the third trimester (Cochrane review) In: The Cochrane Library. Oxford: Update Software; 1998.
- [Google Scholar]
- Labor induction with intravaginal misoprostol versus intracervical prostaglandin E2 gel (Prepidil gel): Randomized comparison. Am J Obstet Gynecol. 1995;173:1137-42.
- [CrossRef] [Google Scholar]
- Induction of labor, ACOG practice bulletin No. 10 November 1999, Clinical management guidelines for obstetrician-gynecologists. Obstet Gynecol. 1999;94:1-10.
- [Google Scholar]
- Comparison of 25 and 50 microg vaginally administered misoprostol for preinduction of cervical ripening and labor induction. Gynecol Obstet Invest. 2002;53:16-21.
- [CrossRef] [PubMed] [Google Scholar]
- Sample size determination In: Research Methodology and Dissertation Writing for Health and Allied Health Professionals (1st ed). Abuja, Nigeria: Cress Global Link Limited; 2009. p. :75.
- [Google Scholar]
- Maternal and perinatal outcomes of induction of labor at term in the university clinics of Kinshasa, DR Congo. Open J Obstet Gynecol. 2013;3:154-7.
- [CrossRef] [Google Scholar]
- Obstetrics outcome and significance of labour induction in a health resource poor setting. Obstet Gynecol Int. 2014;2014:419621.
- [CrossRef] [PubMed] [Google Scholar]
- Statistics review 4: Sample size calculations. Crit Care. 2002;6:335-41.
- [CrossRef] [Google Scholar]
- Trans-cervical Foley catheter balloon versus vaginal prostaglandin E2 suppository for cervical ripening and induction of labor: A prospective randomized controlled trial. Chin J Perinat Med. 2011;14:648-52.
- [Google Scholar]
- Labor induction with 25 microg versus 50 microg intravaginal misoprostol: A systematic review. Obstet Gynecol. 2002;99:145-51.
- [CrossRef] [Google Scholar]






