Translate this page into:
Silicone implant as a potential association with multifocal/multicentric breast cancer: A case report

*Corresponding author: Aqeel Shakir Mahmood, Department of Surgery, University of Baghdad, College of Medicine, Baghdad, Iraq. aqeel.shakir.mahmood@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mahmood AS, Altamee EA, Shakir AA, Sabri S, Al-Qaraghuli AK, Ismail M. Silicone implant as a potential association with multifocal/multicentric breast cancer: A case report. Ann Med Res Pract. 2025;6:2. doi: 10.25259/ANMRP_14_2023
Abstract
Breast augmentation with silicone implants is a prevalent procedure worldwide, although with certain associated complications. While the current literature does not establish a direct causative relationship between implants and breast cancer, there are recognized diagnostic and therapeutic challenges posed by the presence of implants in the event of breast cancer. We report a unique case of a 37-year-old premenopausal woman with silicone breast implants who detected a palpable mass in her right breast. On further evaluation and diagnostic tests, multifocal and multicentric invasive ductal carcinoma was confirmed. Despite the complexity introduced by the presence of implants and multifocal and multicentric disease, which typically directs management towards mastectomy, a decision for breast-conserving surgery (BCS) was reached following thorough multidisciplinary consultation and pre-operative planning. The procedure was successful, with clear resection margins, no intraoperative complications, and preservation of esthetic outcomes. The long-term success of the personalized BCS approach, highlighted by the absence of local recurrence at the 3-year follow-up, underscores the importance of personalized, multidisciplinary planning in treating invasive ductal carcinoma in patients with silicone breast implants. This case underscores the need for further investigation into the potential link between silicone implants and multifocal and multicentric invasive ductal carcinoma, and reconsideration of prevailing surgical approaches to better utilize BCS.
Keywords
Breast augmentation
Breast-conserving surgery
Long-term follow-up
Multifocal invasive ductal carcinoma
Silicone implants
INTRODUCTION
Breast augmentation with silicone implants is a widespread procedure globally. Although silicone implants have been associated with certain complications, current literature does not establish a direct causative relationship between them and the development of breast cancer. However, the diagnostic and therapeutic challenges that implants pose in the event of breast cancer are well-recognized.[1] This case report highlights a complex presentation of multifocal and multicentric invasive ductal carcinoma in a pre-menopausal woman with silicone breast implants, treated successfully with breast-conserving surgery (BCS). The unique nature of this case underlines the need for further research to investigate potential links between silicone implants and multifocal and multicentric breast cancers and adjust clinical approaches accordingly.
CASE REPORT
We present a noteworthy case of a 37-year-old premenopausal woman with a history of silicone breast implants who detected a palpable mass in her right breast. Initial clinical evaluation revealed a firm, non-mobile mass. Subsequent magnetic resonance imaging showed multifocal and multicentric rim-enhancing lesions – a breast imaging-reporting and data system V categorization, suggestive of malignancy [Figure 1]. A subsequent ultrasound-guided core-needle biopsy confirmed invasive ductal carcinoma, hormone receptor-positive, and human epidermal growth factor receptor 2-negative.
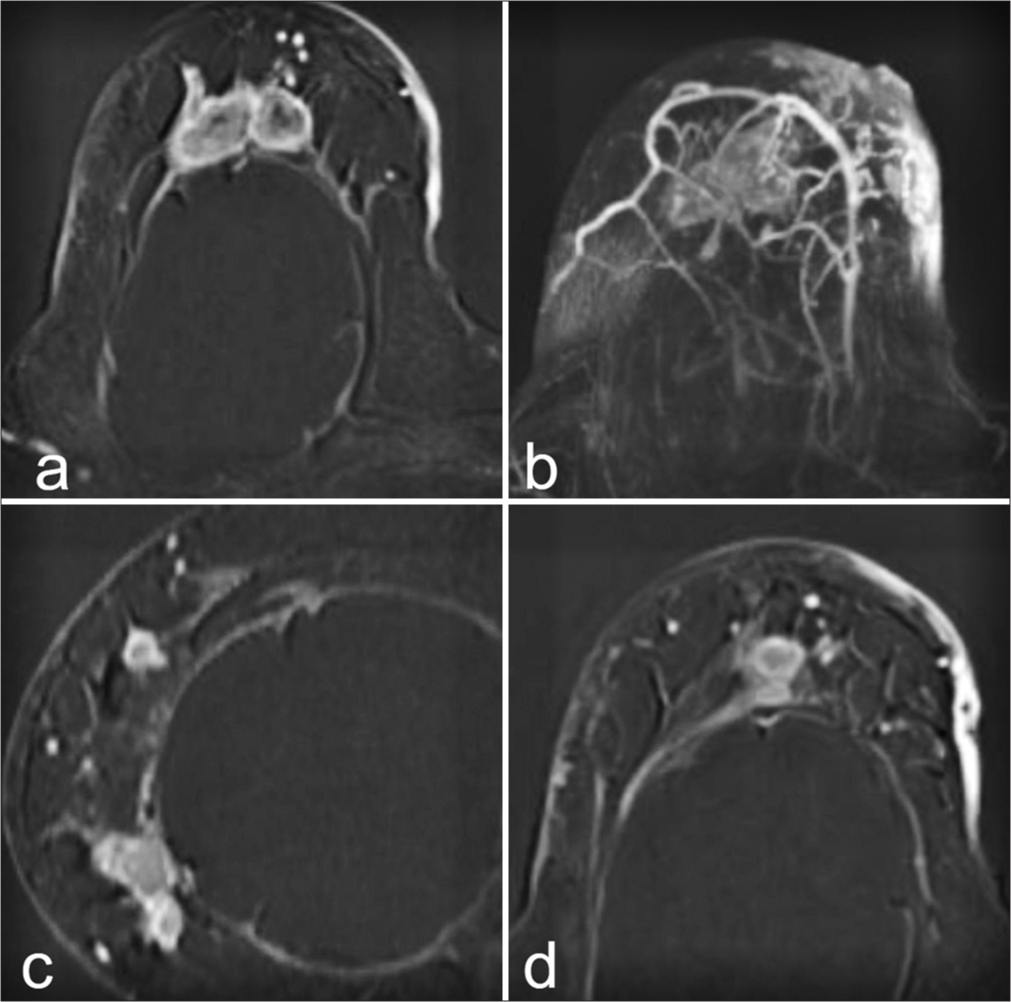
- This is a description of an MRI scan consisting of four images labeled. (a) Axial T1-weighted MRI post-contrast image revealing a well-defined, enhancing mass located in the upper outer quadrant of the breast, exhibiting rim enhancement. (b) This image displays a second, separate mass in the lower inner quadrant with similar rim-enhancing characteristics. The lesion’s distinct boundary and heterogeneous internal structure are indicative of an aggressive, possibly high-grade tumor with necrotic components. (c) The third subpart demonstrates another enhancing lesion in the axillary region, consistent with multifocal disease. (d) The final image captures the multifocal and multicentric nature of the disease, highlighting multiple enhancing lesions across different quadrants of the breast.
The presence of silicone implants and multifocal and multicentric disease usually directs surgical management toward mastectomy due to diagnostic and therapeutic complexities. However, after exhaustive multidisciplinary consultation and detailed pre-operative planning, a decision was made to pursue BCS.
The surgery, which entailed resection of each tumor with an emphasis on clear margins and the use of oncoplastic techniques for preserving esthetic outcomes, was successfully conducted without intraoperative complications. The patient had an uneventful post-operative recovery, indicating a well-tolerated procedure. At a 3-year follow-up, the patient demonstrated no local recurrence, underlining the long-term success of the personalized BCS approach.
DISCUSSION
Concerns surrounding the safety and potential complications of silicone implants continue to circulate within the medical community. Since their inception in the cosmetic breast surgery field in 1962, queries surrounding their potential carcinogenic properties have persisted, culminating in a temporary ban from 1992 to 2006. Given the prevalence of breast implants among American women, exceeding 2,000,000, it is of critical importance to rigorously evaluate their safety.[2]
The possible carcinogenic effects of silicone implants manifest both locally and systemically. There is evidence linking silicone implants to breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL) and breast implant-associated squamous cell carcinoma (BIA-SCC). BIA-ALCL, a T-cell lymphoma, was initially documented in 1997 and the US Food and Drug Administration (FDA) confirmed its rare association with textured breast implants in 2011. BIA-SCC, a unique epithelial-based malignancy separate from BIAALCL, was first reported in 1992, and the FDA subsequently issued a safety advisory in 2022 addressing the potential risk associated with breast implants.[3,4] Furthermore, epidemiological studies have revealed increased risks of cervical, vulvar, and lung cancers in patients with breast implants. However, these risks may be more strongly associated with lifestyle factors, such as smoking habits and sexual behavior, rather than the implants themselves.[5]
At present, no data were to suggest a correlation between breast implants and multifocal and multicentric invasive ductal carcinoma. Our case, however, points to the need for further exploration in this area. Given the limited available data, we can only hypothesize about the etiology of this tumor. Potential mechanisms may include a local inflammatory response triggered by silicone-derived products, specific bacterial species attached to the prosthesis surface (biofilm), possibly through an autoimmune response, or toxic products associated with implant production acting as direct mutagens.[4]
In addition to potential carcinogenicity, the impact of breast implants on the timeliness of breast cancer diagnosis remains a contentious issue, largely due to their radiopaque nature, potentially impeding mammogram interpretation. Conversely, there is a theory that implants might aid in detecting palpable breast tumors, providing a contrasting backdrop for palpation, despite being associated with more invasive cancers.[6]
In Iraq, a particular concern arises from the tendency to opt for mastectomy over BCS, despite consensus in the literature regarding their equivalence and, in some instances, superior survival outcomes with BCS coupled with radiotherapy. Our case reinforces the advantages of BCS in managing invasive ductal carcinoma, as evidenced by the absence of recurrence on follow-up and significant improvements in psychosocial well-being.[7,8]
In summary, our case of invasive ductal carcinoma in a patient with silicone breast implants emphasizes the necessity for further investigation into potential correlations between implants and multifocal and multicentric breast cancers. In addition, the successful outcome reinforces the potential value of BCS as a treatment option, challenging the traditional reliance on mastectomy in similar complex cases.
CONCLUSION
This case underscores the importance of personalized, multidisciplinary planning in treating invasive ductal carcinoma, even in the presence of silicone breast implants. The potential link between silicone implants and cancer warrants further investigation, particularly in cases of multifocal and multicentric invasive ductal carcinoma. There is a need for reconsideration of prevailing surgical approaches and better utilization of BCS, as demonstrated by the successful long-term outcome in our case.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
Patient consent is not required as patient’s identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Breast implants and breast cancer: A review of incidence, detection, mortality, and survival. Plast Reconstr Surg. 2007;120:70S-80.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer risk among Danish women with cosmetic breast implants. Int J Cancer. 2006;118:998-1003.
- [CrossRef] [PubMed] [Google Scholar]
- Breast implant-associated squamous cell carcinoma: Initial review and early recommendations. Plast Reconstr Surg Glob Open. 2023;11:e5072.
- [CrossRef] [PubMed] [Google Scholar]
- Breast implants and the risk of anaplastic large-cell lymphoma in the breast. JAMA Oncol. 2018;4:335-41.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship of silicone breast implants and cancer at other sites. Plast Reconstr Surg. 2007;120:94S-102.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of implant location on breast cancer characteristics in previously augmented patients: A systematic literature analysis. J Cancer Prev. 2018;23:93-8.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term quality of life in patients with breast cancer after breast conservation vs mastectomy and reconstruction. JAMA Surg. 2022;157:e220631.
- [CrossRef] [PubMed] [Google Scholar]
- Survival after breast conservation vs mastectomy adjusted for comorbidity and socioeconomic status: A Swedish national 6-year follow-up of 48 986 women. JAMA Surg. 2021;156:628-37.
- [CrossRef] [PubMed] [Google Scholar]







